One of the biggest barriers to improving ICU patient care is a lack of interdisciplinary collaboration, especially when it comes to ICU rounding.
In theory, rounding should give clinicians the opportunity to review and discuss each patient’s care, and then come together to ensure that care is a reflection of best practices and the patient’s wishes.
It should promote effective communication and collaboration, allowing clinicians to work collectively to make more comprehensive and well-informed decisions, while helping teams to identify risks, improve patient safety, prevent errors or inconsistencies, and promptly implement necessary interventions.
Moreover, it should also enhance continuity of care by ensuring every member of the ICU team is on the same page about how each patient is to be treated, allowing for a seamless transition between shifts, and reducing the incidence of misunderstandings or misinterpretations.
Ideally, ICU rounding should also empower patients and their families by involving them in the decision-making process, enhancing their understanding of the care being provided, and giving them the opportunity to ask questions and voice concerns.
This all helps to promote a more patient-centered approach, while building trust, and enhancing the experience, quality of care, and outcomes of patients in the ICU.
But unfortunately, when it comes to ICU rounding, this is not how things usually play out.
The sad reality is, like so many other aspects of ICU culture, rounding routines can be hard to redirect, and this can create dire consequences for clinicians, patients, and the ICUs where they’re treated.
So, if you’re looking to improve ICU patient care by reevaluating your rounding processes, then you should definitely keep reading.
Because in this article, I’m going to explain what needs to change when it comes to ICU rounding culture, and how I and my team can help you to implement those changes.
ICU Rounding Culture: What Needs to Change
Participating in ICU rounding practices is one of the most important aspects of our consulting.
Observing ICU teams during this process allows us to assess how familiar clinicians are with evidence-based practices like delirium management and early mobility in the ICU, and the level of collaboration between clinicians.
At the same time, this also gives us the opportunity to jump in when we feel it’s necessary to address knowledge gaps and opportunities for application of the ABCDEF Bundle.
This allows us to ensure clinicians are following evidence-based practices, and that they understand the importance of these protocols, and how to implement them.
But unfortunately, we continue to find that, in general, the prevailing ICU culture has not normalized a rounding process that instinctively involves the ABCDEF Bundle.
With that in mind, below I’ve detailed several things that need to change when it comes to ICU rounding culture, so you can identify gaps and learn about tools that can help guide your team’s progress.
Not Taking Enough Time

When it comes to ICU rounding, a common issue I’ve seen is that some teams do not allow themselves enough time to conduct thorough rounds.
On the other hand, I’ve sat in on much more comprehensive rounding processes where they make a point of spending a significant amount of time on each patient.
These kinds of ICUs tend to be more on the academic side of things, where medical students or residents present, and attending doctors take time to teach and discuss things at length, often spending several hours completing their rounds.
But a lot of ICU teams are just trying to get through their patients as quickly as they can. Shockingly, sometimes they spend no more than 30 minutes on the entire process for 20 or more patients.
This kind of assembly line approach is not good for patients, as it does not provide enough time to discuss the many concerns related to critical illness, consider the humanity of each patient, or take a comprehensive look at each patient’s care.
Moreover, this also makes it pretty easy to overlook life-threatening issues, along with opportunities to educate and develop your team.
Ideally, the process should include all the key disciplines of your ICU team, including doctors, nurses, pharmacists, physical therapists and/or occupational therapists, dietitians, social workers, family members, and anyone else who is involved in the care of your patients.
The presenter should walk the team through all of the details related to each patient, including their name, age, why they were admitted to the hospital, the course of events that brought them to this point, their current condition, and what can be done to improve their care.
This requires careful consideration of several different aspects, including things that many ICU teams tend to overlook, like whether the patient is suffering from delirium, along with their CAM and RASS scores, level of sedation, level of mobility, and any barriers to mobility that they might be experiencing.
Then, once all of this has been discussed, the team can work together to determine if anything can be done to improve the patient’s care and implement any necessary interventions.
Lack of Collaboration
Lack of collaboration between clinicians is one of the biggest problems with ICU rounding culture.
It’s easy to skim through presentations quickly and try to get the whole thing over with as soon as possible. But it’s much more beneficial to build an environment that allows clinicians of each discipline to have a fair opportunity to provide suggestions and offer their expertise.
That being said, multidisciplinary rounds can actually be a lot different from interdisciplinary rounds, which allow for true collaboration.
Interdisciplinary rounds happen when collaboration is warmly welcomed and proposals from colleagues are sincerely discussed, valued, and taken seriously.
But unfortunately, this is not how things tend to go when it comes to ICU rounding.
More likely, what will happen is something like this: A progressive physical therapist will be brave enough to suggest mobilizing a patient, but members of the ICU team, who don’t understand the ABCDEF Bundle, will respond by saying something like, “They’re still intubated, so we can’t,” or “They’re still sedated and they were too agitated during the last SAT this morning.”
But a team that truly understands the ABCDEF Bundle will use its rounds as an opportunity to bring each discipline together to develop plans on how to keep each patient as awake, mobile, and free of delirium and ICU-acquired weakness as possible.
For example, if a nurse reports that a patient has been sedated, a pharmacist may ask, “Is there an indication for sedation?”
And if the nurse responds by saying, “When we tried to turn it off, the patient became agitated and we turned it back on,” this provides an opportunity for a physician to ask, “Does the patient have delirium? And how can we turn the sedation off?”
Then, when a physical therapist says, “Let’s get the family to the bedside, and I would love to help you turn the sedation off and get the patient up,” the team will be much less likely to be hesitant about this suggestion, as they’ll understand the evidence, and how that approach can benefit them, the patient, and the ICU as a whole.
This method of ICU rounding encourages discussion and makes it more likely that clinicians will accept each colleague’s contribution to that conversation, and remain open to their suggestions, allowing everyone to be on the same page, and the load of patient care to be shared.
In addition, this allows ICU teams to make decisions regarding sedation, delirium, and mobility based on evidence, rather than culture and fear.
With that in mind, we make a point of always having a seasoned respiratory therapist and physical therapist with us while we’re on-site, because not only can they offer their expertise on these practices, and how to improve the rounding process, but this also helps us to reinforce the interdisciplinary approach and remind clinicians of the importance of all this.
We also make sure to train whomever is leading the rounds to create an environment that facilitates this kind of discussion, and provide them with a toolkit to ensure every member of the ICU team is prompted to follow this systematic approach to rounds.
At this point, it’s also important to mention that there is significant evidence to show the benefits of interdisciplinary collaboration during the rounding process.
For example, one study, which looked at the impact of allowing pharmacists to participate in multidisciplinary rounds, found a long list of potential benefits of this kind of collaborative approach.
The study found that allowing a pharmacist to perform daily sedation management for patients “resulted in fewer hours of patient exposure to continuous sedation, with an overall 46% reduction in continuous infusions of sedatives and reductions in both ICU and total hospital LOS, resulting in estimated savings of $1.2 million in direct hospital costs and $183,216 in drug costs.”
In addition, it found that allowing pharmacists to collaborate with ICU teams using the practices outlined in the ABCDEF Bundle offered “improvements in several outcomes, including mean ventilator days per patient, ICU LOS, and mortality.”
Not Digging Deep Enough
Another issue with ICU rounding culture is that teams may not dig deep enough to actually understand the barriers and needs of each patient.
This happens mainly due to a lack of understanding of evidence-based practices like delirium management and early mobility in the ICU, along with communication breakdown between clinicians, which is exacerbated by poor rounding practices, such as imposing strict time limitations.
For example, a nurse may report, “The patient was agitated and failed their SAT,” which means that sedation was resumed. But oftentimes, this is as far as the conversation will go, and the rest of the team will accept sedation as essential for that patient and something to address later on when it’s time to think about extubation.
However, a team that understands the ABCDEF Bundle will dive much deeper, and a colleague might ask questions like, “Why was the patient agitated? Were they in pain? How are they communicating? Do they have delirium? And was their family present during that awakening trial?”
Then, if the nurse confirms, “They’re CAM positive,” the physician can use that as an opportunity to help educate their team, and encourage them to make delirium, agitation, sedation, and mobility a priority.
At this point, a physician on this type of team might say something like, “This is acute brain failure. Sedation is likely causing, exacerbating, and prolonging their delirium. And for every one day of delirium, there is a 10 percent increased risk of death. This patient needs to have sedation turned off, and be mobilized, with their family present, while having their sleep prioritized.”
They can then ask the physical and/or occupational therapists to accompany the RN and RT to help with the awakening trial and promptly mobilize the patient with the goal of turning off the sedation.
This may also prompt the physician to join their team at the bedside during the awakening trial and help assess causes of agitation, such as pain, fear, or delirium.
These kinds of moments during rounds can be the difference between a patient being awake, mobile, communicative, and thriving, or continuing down the path of sedation, immobility, and the many complications that follow.
In any case, doctors need to have a deep understanding of delirium, ICU-acquired weakness, post-ICU syndrome, early mobility, sedation management, and the ABCDEF Bundle.
This expertise will help them orchestrate masterful collaboration for their teams by diving deep into the evidence, while considering the humanity and best interests of each patient.
Failing to Involve Family
I am also a strong proponent of involving patients’ family members in the rounding process.
But in my experience, ICU clinicians can have strong reservations about having families present during rounds. It seems to go against their culture, makes them feel uncomfortable, and even vulnerable to have families involved in the rounding process.
Much of this stems from a lack of understanding of the role and value of the family as key players in a patient’s survival in and outside of the ICU.
But the truth is, involving patients’ families in the rounding process offers many benefits, including:
- Improved communication: Involving family members in ICU rounding facilitates open and transparent communication between healthcare providers and the patient’s loved ones, allowing for discussions about the patient’s condition, treatment plan, and progress. Their involvement promotes a better understanding of the situation, reducing anxiety, and helping to manage expectations.
- Enhanced patient-centered care: Family members can provide valuable insights into the patient’s medical history, preferences, and values, and their presence during rounding ensures that the care plan aligns with the patient’s individual needs and wishes.
- Emotional support: The ICU can be an overwhelming and stressful environment for both patients and their families, but allowing family members to participate in rounding offers emotional support and can alleviate anxiety and foster a sense of trust in the care being provided.
- Shared decision-making: Inclusion of family members in rounding promotes shared decision-making, and involving the patient, their family, and the medical team can lead to more informed choices and increased satisfaction with the care provided.
- Education and empowerment: ICU rounding provides an opportunity for family members to learn about the patient’s condition, prognosis, and ongoing care needs. It allows them to ask questions, seek clarification, and receive education about the patient’s treatment and post-ICU care.
- Continuity of care: Involving family members in ICU rounding promotes continuity of care, as they become familiar with the patient’s care plan, which can be helpful when transitioning from the ICU to other healthcare settings or when managing care at home.
How We Can Help You Improve Your Rounding Process

When we work with your ICU team, we start by encouraging everyone to participate in our series of webinars, so they can better understand the why and how of the evidence-based practices in the ABCDEF Bundle.
Then, once we arrive on-site, the first step is to simply observe your current rounding process.
This allows us to see who is present during rounds, who is presenting, what kind of order or systematic approach is being used, which aspects of patients’ status and care are discussed, and how the team makes decisions.
After assessing all these aspects, we’ll work with your team to make your rounding process more succinct, thorough, and efficient, while ensuring delirium management, pain management, sedation, RASS, communication, family engagement, and early mobility in the ICU are included in the discussion.
The goal is to help your team have the understanding, tools, and team dynamics to apply the principles of the ABCDEF Bundle to your rounding process using a collaborative approach that optimizes each discipline’s expertise to ensure the best patient outcomes.
By the end of our training, each team member will understand why keeping patients awake and mobile is so important, along with how to go about doing this in the safest way.
What’s more, they will know how to discuss concerns and barriers during rounds and work together to develop a plan to overcome the unique challenges of each patient with the goal of giving patients the absolute best chance to walk out of the hospital doors, discharge home, and resume their normal lives.
Each team member will also learn the importance of a collaborative approach, and the value of each discipline’s contribution, while being equipped with a systematic method, based on the principles of the ABCDEF Bundle, which allows them to work with their team to provide the best possible care for each patient.
As part of that process, we also provide clinicians with a rounding tool, similar to the ICU rounding sheet shown below, which comes from the University of Colorado ICU and is actually based on the evidence-based practices we espouse.
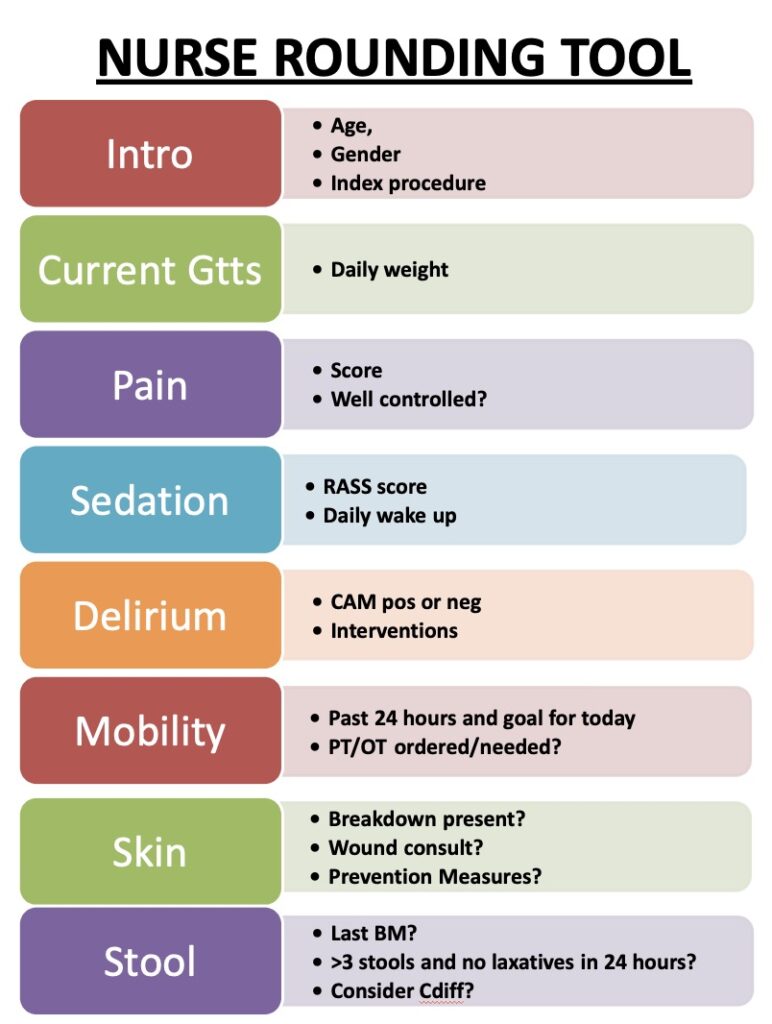
This ICU rounding sheet will help to ensure that what we teach is not forgotten, and will go on to become a standardized part of the rounding process followed in your ICU.
Evidence shows that using this kind of tool can provide a multitude of benefits for any intensive care unit.
For example, one observational study found that implementing this kind of tool “can result in improvements in engagement of nursing staff and in overall communication.”
Another study looked at whether time allocation issues in the ICU could be solved by using a rounding tool, and it found that the use of these tools “potentially mitigates disproportionate time allocation and communication breakdowns during rounds,” with one tool “almost completely eliminating such effects.”
All things considered, ensuring that clinicians use this kind of ICU rounding sheet is integral to the improvement of the ICU rounding process, as it reinforces the importance of considering these aspects of patients’ care, and makes the implementation of this process more sustainable.
What’s more, once it becomes standard practice, and part of your ICU culture, clinicians will appreciate the benefits it provides to your team, your patients, and your ICU as a whole.
Do you want to improve the rounding process in your ICU? We are here to help! Let’s discuss your team’s needs. Contact us here.




