SUBSCRIBE TO THE PODCAST
The ICU is not a very warm and welcoming place, so in this episode Kali gives you a quick tour into the intensive care unit and the ICU team.
Episode Transcription
Welcome to the ICU. You likely don’t feel so welcome. It’s not a very warm and welcoming place. No one chooses to go there except those that volunteer to work under difficult conditions in stressful and heartbreaking situations. You didn’t sign up for this… yet here you are. It’s a whole new world in here. So let me give you a quick tour.
The intensive care unit is a specialty of medicine dedicated to patients that are sick enough to require extra observation and or extra care. Within this specialty, there can be many kinds of ICUs such as trauma, respiratory, or medical surgical. Different hospitals have different levels of ICUs. Not all ICUs have doctors specifically trained for ICU, called, “intensivists”. Smaller and more rural hospitals may have regular hospital doctors called “hospitalists” care for their ICU patients that are not severely ill.
Yet, in normal circumstances, meaning, before the COVID crisis, if a patient required a higher level of treatment, they were sent to a bigger hospital that has the equipment and trained staff to care for the specific illness and level of severity of that patient’s condition. So, being in the ICU naturally causes panic, but even within the ICU, there are different levels of critical illness.
No one wants to be in the ICU, but the ICU really has some significant benefits and I have seen many patients hesitate to leave. For example, in the United States, one ICU nurse has 2 patients. On the normal hospital floors, nurses have 4-8 patients. If the patient is exceptionally ill and in a severe crisis, then the nurse will only have them as their 1 patient. Again, under normal circumstances. In other countries such as Denmark, their ICU nurses have 1 patient all the time. So, being in the ICU means that there is closer and better care for patients in the greatest danger.
Let me introduce the team to you. As I mentioned, the team lead is usually an “intensivist”. This is a physician that has specialized in the ICU, and often in pulmonology or anesthesiology as well. In the states, to become an intensivist, you have to complete your bachelors, then 4 years of medical school, 3 years of residency, then 2 years of fellowship, and then an additional 1 year of fellowship in critical care. This is a total of at least 14 years of higher education and training. Your intensivists likely have years to decades of experience beyond that.
Then you may have a nurse practitioner, or an “NP”- which is someone that has their bachelors in nursing and then years of experience working as a nurse and then went on to get their masters or doctorate. They work alongside the intensivist to develop diagnosis, plans, and procedures as well as collaborate with the team to ensure optimal care for your loved one.
You may have a physician’s associate known as a “PA” who has their masters and years of training and experience. They work alongside intensivists and NPs to also diagnosis, provide plan of care, orders, and perform procedures.
You will have respiratory therapists caring for your loved one. They have their bachelors or masters in respiratory therapy and the expertise in all things oxygen delivery, lungs, and ventilators. Ideally they should care for only 4 patients on ventilators, but they have been a hot commodity during this pandemic and are spread very thin and are taking on far too many patients. Treat them well.
Your nurses have their bachelors or masters and often have additional education and training to be certified as critical care nurses. Many are well seasoned, traveled, and knowledgeable. They are in charge of all of the details and coordination of patient care- from the bathing to medications, tests, mobility- they are the guardians and pulse in the ICU. Again, in the states they should only have 2 patients, but times are hard right now. Care is impacted by how many patients they have. So please, be patient with them.
Physical therapists “PT” should be heavily involved in your loved one’s care right away- we will discuss that more later. They usually have their doctorates in physical therapy and can even specialize in acute care and be additionally trained for intensive care. They are in charge of keeping your loved one mobile, functional, and able to discharge home with you from the hospital. You want and need them there. If they’re not there- ask for them. They too are in high demand right now.
Occcupational therapists have their masters or doctorates in occupational therapy. They are in charge of cognition, fine and gross motor skills, communication, mobility, self care- so many things. They too should be involved right away.
Speech language pathologist have their masters and are in charge of communication, cognition, and swallow. They are the secret weapon of the ICU and a huge player in getting your loved one home. These rehab services, PT, OT, and SLP- are the delirium sWAT team- which we will discuss in another episode. They are under staffed and underutilized in the ICU but will be your best friends in keep your loved one human at this time. You have every right to request them.
Pharmacists are the man behind the veil making so much magic and safety happen. They have their doctorates and often extra residency and certification in critical care. You will probably see them at rounds. Give them an extra high-five. They have been under incredible stress during the pandemic. We would all be in grave danger without them.
Registered Dieticians are also the discreet saviors in the ICU. They have their masters degrees and can specialize in ICU. Their interventions truly save lives. Please make sure your loved one has a registered dietician consultation- no matter how sick they are. You want these geniuses monitoring them and preventing them from getting sicker.
Critical Care techs- This is the fuel of the ICU. They are CNAs that are specially trained for the ICU to make sure foleys are clean, baths are done, rooms are stocked, patients are walked, hair is braided- they are SO busy and so great.
Chaplains can be key players- they have their masters in providing spiritual support. They can be secret weapons for delirium or crisis. Please use them.
Social workers- they have their masters and keep everyone afloat and make sure patients have support they need to succeed after the ICU.
You may also be working with fellows or residents that are doing their training to become intensivists.
Then there is you- the family member or loved one. Your expertise is your loved one. You bring so much to the table. Understand everyone’s roles so you know how to respect and utilize them.
Many of these disciplines will meet together for a daily meeting called rounds. There they will discuss your loved one’s case and collaborate together to develop a plan of care. Hopefully you will be invited to participate in rounds. If not, ask if you can come. It is a good opportunity for you to listen in and write down questions to ask later during the family meeting.
I know, it’s a lot. A lot of people, a lot of different roles, a lot of information. Then you look around the room, and you see so many different machines, monitors, and equipment.
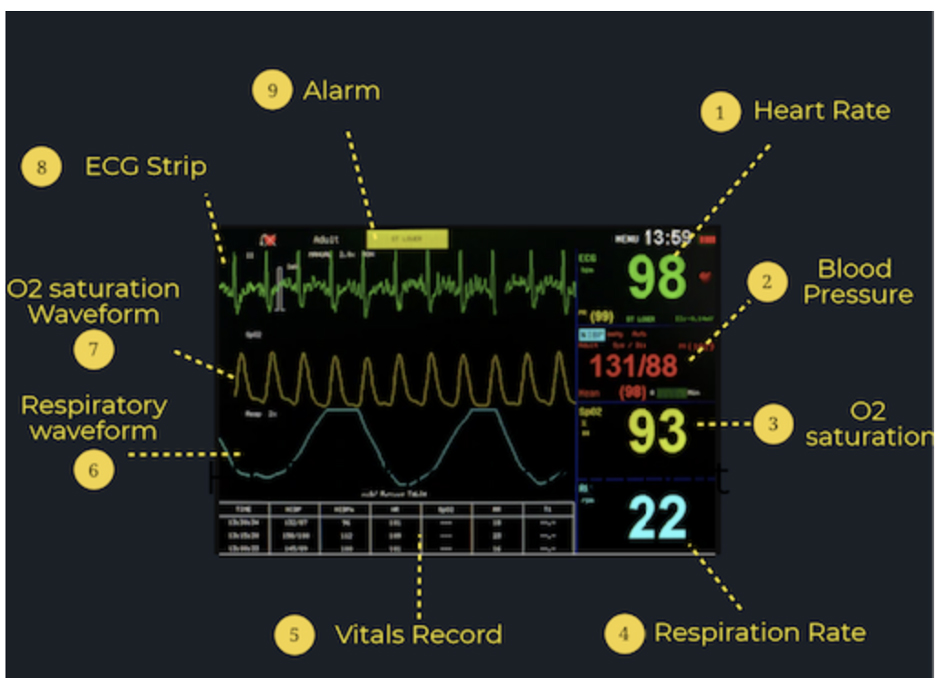
Let’s look at the monitor- the main big screen with all the different lines, colors, and numbers. I would describe and explain it to you, but they can all be so different, I don’t want to make it confusing. Usually, the top lines and then number are for the heart rate. This is reading the stickers on your loved one’s chest. The ICU team will watch the patterns of the heart monitor to look for signs of abnormality or danger. They measure this formally and closely throughout their shift, every time they go into the room, usually when they sit down to chart they can see a monitor by their computer, in the break room, and at the nurses desk. Your loved one is constantly being monitored. They set alarms on the monitors so if something changes outside of normal parameters- everyone will know and they will react.
On that monitor is also the oxygen level monitoring that is being read by a clip or sticker stuck to your loved one’s finger, toe, ear, or forehead. If that falls off, an alarm will sound, and someone will come to help. There often a line and number for respiratory rate- the measurement how many times they breathe a minute. This is usually inaccurate on the monitor, so they’ll usually take it off. It’s ok, they’ll still be monitoring their respiratory rate every 2 hours and probably every time they go in the room. There may also be a temperature reading on the monitor being tracked in the urinary catheter or breathing tube.
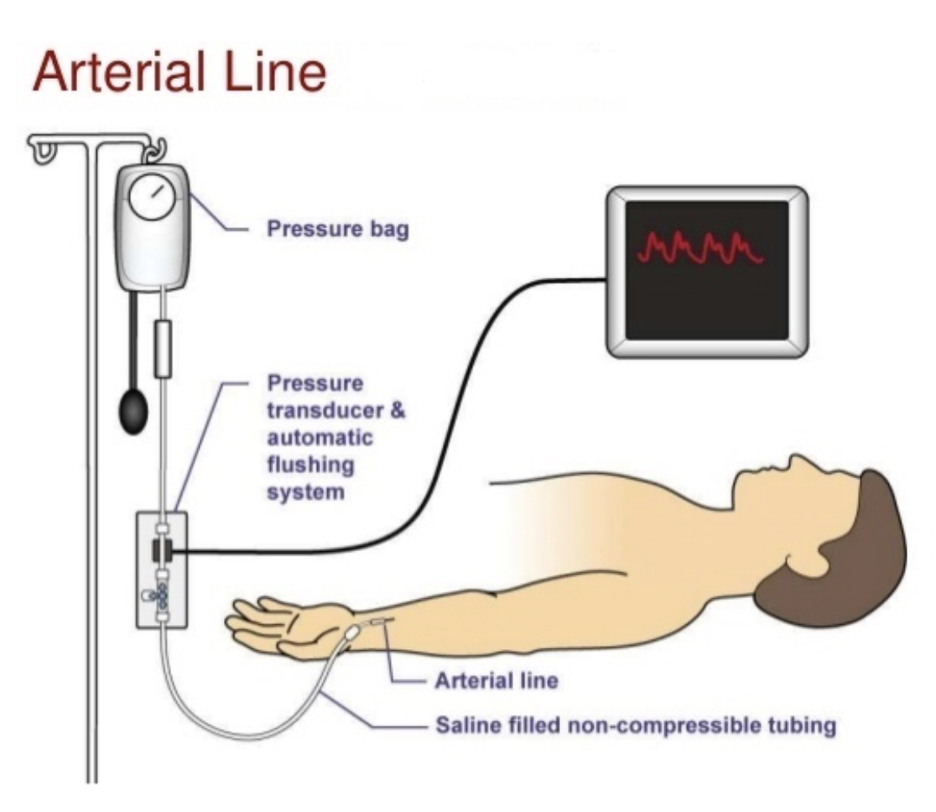
There will also be a blood pressure reading. This will either be from a blood pressure cuff on their arm or from a little catheter in one of their arteries.
Sometimes there are extra readings, but I will just stick to the most common ones for now.
Those numbers may look really overwhelming- but that’s pretty much it. Usually, it’s the heart rate, breathing rate, oxygen level, temperature, and blood pressure. Check out the blog for a visual explanation.
I will do a separate episode later on the ventilator, in case it is not relevant to your loved one’s situation right now.
When clinicans come into the room, and it looks like they’re just coming to check the urinary catheter or give a medication, yet your clinicians are always innately assessing your loved one closely. So, don’t panic. You don’t need to sit and watch the monitors. Even when no one is in the room, they are aware of them and someone is watching the monitors. They are tracking everything that goes in and goes out of your loved one. They are combing through their lab values. They are documenting their behavior, demeanor, sleep, position, and status every 1 to 2 hours.
Yet, you can be part of the observation. You can watch for signs of pain or anxiety. You can help the rest of the ICU team understand how to communicate with them if they are on the ventilator or unable to do so verbally. You know your loved one, you know when something is different or off, and you can help bring awareness to changes.
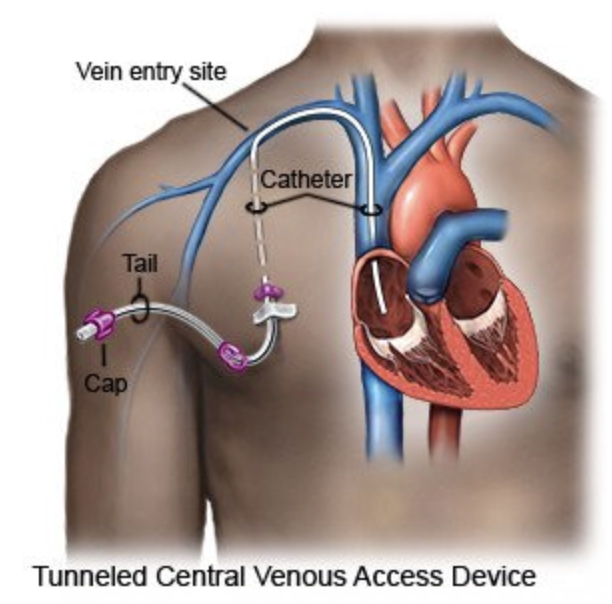
It may be hard to see so many tubes and lines in your loved one. They probably have IV lines- little tubes that go into the smaller veins of their arms, hands, and maybe neck. If it was hard to get access to those little veins or they needed a lot of medications, fluid, or blood, they probably have a central line. This is a bigger tube or catheter that goes into one of the bigger veins in by their collarbone or neck and feeds straight into the heart.
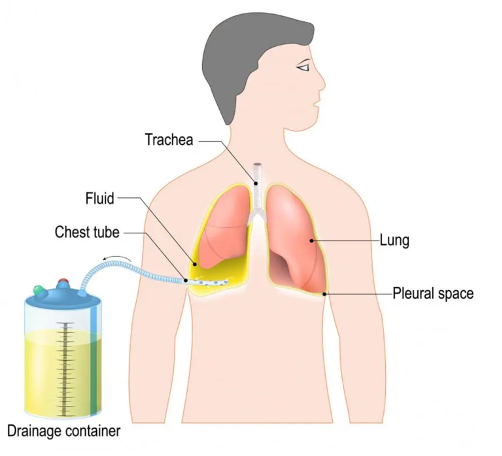
This is a great invention as it allows the ICU team to give a lot of really important drugs really quickly and take effect rapidly. They may have an arterial line- a little catheter into the wrist or groin that goes into an artery and measures the blood pressure with every beat of the heart. This helps the team to keep a really close and usually accurate eye on your love one’s blood pressure second by second. They can also draw blood from the arterial line to run important tests. They may have a chest tube, or different drains which will be shown on the blog.
You can help keep these important lines and tubes safe and in place. If your loved one is confused, make sure they don’t accidentally pull any of those out. The safer you can keep your loved one without the ICU team sedating them, the better they will get and the sooner they will be out of the ICU. As the team gets your loved one out of bed to walk, you can probably help push an IV pole or a wheelchair. These tubes and lines will be less scary as time goes on and you will become familiar and adjusted to them.
Your loved one will stay in the ICU until they are stable and safe enough to go to the medical floor. This usually requires that their blood pressure be consistently normal, they are oriented and not severely impulsive, bleeding is resolved if was present, they do not need more than 5 or 6 liters of oxygen, and they are past the critical phase of their illness and not expected to be at danger of becoming sicker.
They will then be moved to a medical floor where they will be cared for by a nurse that has about 6-8 patients. Your presence will still be helpful during that time.
So, there you have it. That is a brief rundown of the ICU. Ask questions, get informed, and be updated. Stay tuned for the next important episode on medically-induced comas.
ICU MONITOR:
Resources Referenced:
Other Introduction to the ICU: https://www.esicm.org/patient-and-family/
SUBSCRIBE TO THE PODCAST