SUBSCRIBE TO THE PODCAST
How can occupational therapists help decrease time on the ventilator and time in the hospital? How can they preserve function and quality of life? What skills do they bring to preventing and treating delirium? Why should they be promptly utilized in a patient’s journey? Corinne, Mallory, and Rachel share give us insight into the value occupational therapists bring into the ICU.
Episode Transcription
Kali Dayton 0:00
I am so excited to jump right into the glory of occupational therapists. They bring so much knowledge and expertise to the table. And they just need us to remove sedation from blocking their way and let them work their magic. Corinne shares with us one of the many examples into how occupational therapist can drastically change outcomes and the ICU.
Corinne, OT 0:57
Hi, my name is Corinne. I’ve been a critical care OT for four years primarily in the CVICU and MICU. I’m lucky to work at a hospital that allows me to practice at the most advanced levels of my license and allows me to give those patients their ability to be active participants in their care by educating staff on the benefits of decreasing sedation and involvement a therapy for early mobility.
Recently in the MICU, I had a 65 year old male patient that had been intubated, sedated for eight days. They excavated him and he was immediately re intubated, sedated within 30 minutes. The team was planning on trach and pegging him and sending them off to an L tech. I asked two doctors about turning off sedation and allowing therapy to get involved. They said “no, it was too risky. He’s gonna pull on his tube out”. After I pleaded my case. The third doctor said “Okay, let’s give it a shot.”
The nurses were all on board with this. The patient’s wife was at bedsides can help keep the patient calm and not pulling out his lines. Day one of therapy involvement. I set the patient up at edge of bed with help from the nurse and RT, he was able to sit up for about five to six minutes. His SATs were better than they had ever been.
Day three, the patient was able to stand at the edge of the bed twice for about three minutes. On day five, the patient was able to take a couple steps over to her recliner. Two hours later the patient was able to be excavated. On day eight, the patient was transferred to the regular floor on three liters of oxygen was able to walk about 30 feet with a walker.
On day 14, the patient was able to discharge home and no oxygen and using no assistive device. The family was eternally grateful for the one doctor that said yes, that gave the patient his voice and ability to maintain his independence. I think as OTS we have a unique perspective of being able to see the patient as a whole and help with coping and cognition as well as addressing their functional needs. When it comes to the ABCDEF bundle.
I feel that ot plays a key role in multiple parts. As OTs, we can help combat delirium, which is often a huge barrier when it comes to decreasing sedation and weaning to activate. As delivers patients are more likely to pull out their tubes need one on one care than a patient that has cam negative observation and able to participate in their own care.
Another area that OTS play a big roll on is early mobility. As OTS we are just as capable of mobilizing a patient as a physical therapist. On some occasions, I do choose to defer mobility to PT, as the patient may have other ot concerns like their cognition or helping talk a patient through their anxious feelings, and teach them coping skills to help with processing all the events that have taken place. The final component that I feel that ot has a key role on is family and engagement and empowerment.
Family involvement is very important to a patient’s recovery. I feel like when a patient who is can negative not sedated and able to participate in their care, family tends to spend more time at the bedside. I’ve talked with family members of patients that are sedated to arrest a negative three to negative five. And they often expressed that it’s hard for them to see their loved ones in this state, I will often give them ideas of things to do to help them interact with the patient. But I feel like they never stay at the bedside as long as families do when their loved one is awake and alert.
As OTS we can help change the outdated practice of heavy sedation, to a culture of early mobility in order to improve patient outcomes and quality of life. And overall eases the burden on staff because a patient that can move on their own makes everyone’s lives a lot better.
Kali Dayton 4:31
Now let’s talk about delirium management and occupational therapy. Often the cultural response to hyperactive delirium is manifested by agitation is to deeply sedate the patient. Unfortunately, this is often continuing the same thing that is very likely the main cause of the delirium and agitation and prevents actual treatment for that acute brain failure we call delirium.
Yet this is a hard conversation to have, as we are In the midst of a terrible staffing crisis, and nurses especially, are expected to wean off sedation after days to weeks of sedation, and to be the ones to deal with the delirium. This is not only unfair, but it is often impossible amidst the many responsibilities of the RN and the crisis we are in. This is a big reason why I advocate for avoiding sedation and preventing delirium right away, unless we have specific exceptions.
Yet if that is not an option, or if a patient has already been delirious for other reasons. OTs, PTs and SLPs are powerful tools to keep them safe from sedation and help them through delirium. Their involvement is not to be delayed. We have highly trained experts available, who are often unrecognized and under appreciated. Occupational therapists have their masters in the art of preserving function, including cognition and mobility. Let’s dive deeper into the role that occupational therapists should have in the ICU. And why they should be in the ICU, not just visiting the ICU to best utilize their services, we must understand what skills and expertise they bring. Rachel Mallory, thanks so much for coming on. Do you guys mind introducing yourself?
Mallory, OT Student 6:15
Yeah, my name is Mallory. I am the Capstone student at Ohio State University. I’m studying occupational therapy.
Rachel, OT 6:23
And my name is Rachel and I’m a critical care occupational therapist. And I am Mallory’s mentor.
Kali Dayton 6:31
And I am so excited to have you guys on it’s just funny, throughout the podcast, I’ve been saying, “Get OT in there! Get OT in there!”- but I don’t think that I’ve really covered, adequately, what ot does. What do you bring to the bedside? And why do you need to be in there so promptly, especially when it comes to obviously, mobility, functional status and delirium management?
So tell us and again, the roles the scope of practice seem to vary by state by facility by team. So let’s talk about what can and should be for OTs, why teams need to expand their utilization and role for OTs and give you guys all the reins to use your license. So what is OT’s role in the ICU?
Mallory, OT Student 7:20
Yeah, that’s a great question. Thanks for bringing that up. So occupational therapy is a role in general is we start by doing a chart review on the patient and evaluating their medical status. So we look at their current physical and cognitive functioning, as well as how they were doing before their hospitals. So when we go in the room, we kind of see what their current status is right now, and help set a plan of care for how we can help them in the future.
And basically, our role as occupational therapist is to help our patients live their life to the fullest. So this can mean helping them overcome any functional, physical, cognitive, social, emotional barriers to doing their everyday life. So it really depends on the patient what we’re actually doing, but it can look very different from patient to patient, but the overall goal is always going to be the same.
And in the ICU, our patients are often pretty critically ill, right. So we’re not going to be doing maybe those things that you’ll see patients doing and out how outpatient like meal preparation or home management, stuff like that. So we’re starting with more of like the basic activities, and we definitely have a really strong role and presence in delirium management as well. So that is something that we’re always looking at when we’re going into the patient’s room.
Rachel, OT 8:33
Right. I think a lot of times people just think that all we focus on are activities of daily living, and also often confuse us for physical therapists. But I like to think of us doing those things, but also the three C’s, which which consider cognitive communication and coping. And within that cognitive component is the delirium component as well.
Kali Dayton 8:58
Yeah, I think occupational therapy is just miss misunderstood across the board, right? My daughter has been doing a lot of occupational therapy, like four times a week. And it’s been amazing to see how they involve the neuro system, and they’re working on her reflexes to functional things to sensory to just, your training is so vast, that watching how they’re doing it, you know, in the development of delayed pediatric patient, yeah, how valuable that can be, especially in the setting of delirium. And what do you do for delirium? Like, why should you be head of the delirium SWAT team?
Mallory, OT Student 9:40
That is a really good question. So there’s a lot of reasons. One thing that we often think about is we’re one of the few professions if not the only profession that gets to spend an extended period of time in a patient’s room with them, and really get to know them and get to address the delirium as part of our job right. So we’ll be in there sometimes up to like an hour. Yeah, we’re working with the patient the entire time. And we’re implementing, like delirium prevention or delirium reduction techniques that are evidence based.
And this is what I’m doing my capstone project on, actually. So there’s a lot of different things practically that we can do for delirium. So some things would be like reorientation, which seems pretty basic, but will often add environmental cues to the patient’s room to help them be more oriented to what’s going on around them. So almost every day, we’re putting up signs in the patient’s room, your name is blank, you were at the hospital for this surgery.
And then we have a sign that says today is and we provide them with the month in the year and the day that it is we also have a day and a night sign that we have provided with nursing staff so that they’re able to switch it over. Because as you know, it’s really common for delirious patients to think that it’s nighttime during the day. And we’re, we’re in there working with them for therapy, and you ask what time of day do you think it is, and they say, oh, nighttime, and then really, Okay, gotta go run and get one of our signs.
And you know, cue them to look at the windows and look at the signs and the different tools that we’ve provided them with. So environmental modification is one thing, the research also supports, functional mobility is important. So OTS can also play a role in functional mobility, so we won’t just get somebody up to stand them, but we’ll get them up with a purpose, right. So to help them progress to something like a toilet transfer, or to help them stand while they’re doing a functional activity. So we also do play a role in that. And we work with the physical therapists in the in the way of functional mobility as well.
But some other things that we can do for delirium would be helping people with coping and communication. So as you know, the ICU can be a really traumatic environment for a lot of people. So we’re also one of the only professions that can sit down with them, and listen to them and talk to them for an extended period of time about how they’re actually doing, and how their medical status is affecting their day to day life. Right. Because like, that’s our goal is like to help them overcome those barriers.
So our role in delirium management can look like a lot of different things for different people. But like the goal of OT is like, we want to make our intervention specific to that individual. And we want to cater what we’re doing to a specific person, rather than trying to fit everybody into like, you know, a mold. So we really consider the person and their wants and their needs and their support systems that they have around them. So it’s kind of hard to define because it is so broad, but the general principles that are supported by the research would be cognition, mental health and coping, physical physical activity, which includes early mobility, as well.
Kali Dayton 12:42
So I’m just thinking, What a powerful tool you are for delirium. I think, currently, our culture is often if we see signs of delirium, especially someone’s on mechanical ventilation, the agitation, confusion and ability follow direction. Right now the instinct is to sedate them deeper. And if we really understood those tools for delivery management, especially how experts the expertise that you have, instead of hitting the station, again, rather calling you in to work with them, how drastically different outcomes could be just delirium doubles the risk of mortality, for every one day of delirium, there’s a 10% increase the risk of death.
I mean, if we thought that way, if we were that panicked about delirium, understanding, okay, this increases the chances of dying and having long term psychological and cognitive impairments, you guys would be so busy and super high demand, because you’d be probably every room in the ICU.
Mallory, OT Student 13:44
Yeah, that’s a really good point that you brought up that instead of deferring to sedation that, if you know, people better understood that occupational therapy isn’t just for ADLs, or when patients are ready to do ADLs. It’s for those patients who are agitated or who might be slightly sedated, but they could really use us. And I feel like, like you said, we would be utilized to our full capacity in the ICU.
And I think my mentor does a really good job about communicating with the nursing staff and kind of, you know, talking to them about like, why the patient’s agitated if they are agitated, and then we can go in and work with them. And something we’ve been working on is communication with a lot of our patients in the ICU. So if they’re able to communicate our needs, their needs to us, we might be able to help with that agitation.
Maybe they’re in pain, or they have to go to the bathroom, or there’s something that they need to communicate, that they can just not get across, that’s causing them to be agitated that if you know, we’re able to get to the root cause of that we can, you know, help just alleviate that just a little bit rather than them going back on sedation. And I think it goes the other way too. So sometimes we think of like, agitation and delirium, but also that like hypoactive delirium as well that is less identified in patients.
So being maybe like So one of the disciplines that goes in and recognizes that, and that we can help those patients be more responsive in therapy as well. And use, we use a lot of like poly sensory stimulation and stuff like that, to try to help wake patients up and try to see like, if we can get them to be more responsive. So there’s like both sides that we see, right, we see like the agitation that we also see like the sedation and catering our interventions to whatever their Rask score is, can kind of help, ideally, eventually bring it back to that like zero wrath, right? And hopefully, like, helping them come out of delirium as well.
Kali Dayton 15:39
Oh, this is so great, because it just reinforces how much we need that interdisciplinary collaboration. One of the concerns about avoiding sedation has been in the ICU is that nurses are already so overwhelmed. I mean, they’re, they’re constantly giving life saving interventions, such as the medication, the drips, the procedures, things like that, that sometimes for nurses, the thought of having to communicate with the patient is overwhelming.
Because I don’t have time to even talk to them, let alone to reorient them every time they go in the room, or deal with their agitation. And so sometimes it’s a sense of defensiveness as in, if we change this practice, it’s going to be more work for us. Well, it sounds like what you’re saying is, you’re not alone in this. Yeah, when you avoid sedation, we can actually participate more in their care and be of more help. And this should be easier for everybody. I mean, if you guys help address those root causes of agitation, because nurses don’t necessarily have the time to sit there and with a communication board and try to figure out if they have pain, where’s the pain? Are they scared? Why are they scared? What are they seen in their hallucinations?
They don’t always have that time, or even the training or expertise to do that, unfortunately. But if we understood that you’re the SWAT team for continuing the delirium with sedation, that we can actually treat it with occupational therapy. And as you guys have that kind of communication, that collaboration, where you’re coming to them saying, Why is sedation on what can we do to help get it lower so that we can work with them? What is their? Why is their wrath so low? This is what I’m seeing with the delirium. Here’s a day and night board. That is such a good idea. And but that, again, takes collaboration, right? The nurses have to follow up with it as well. Yeah, how do you see those dynamics working even just within your team?
Mallory, OT Student 17:25
I think we’ve definitely been building stronger relationships with our nurses. So when I arrived at the beginning of my capstone, we just switched over into the cardiovascular ICU. So we were getting to know all of our patients and getting to know the nursing staff working there and everything. And I just think I’m thinking back to a really cool story where so one of our goals is ot on the floor has been to kind of round to every single room and ask ourselves, if this person doesn’t have an occupational therapy eval why?
So they’re like automatic holds for us. So like, if a person is on a neuromuscular blockade, or they have an open chest or their unbelief, Cherie, or they have more than three presses. But if they don’t have one of those automatic holds, we ask ourselves, why and soon, are they going to be ready for an OT, eval? And yeah, so the example that I’m thinking of is we are rounding on the floor. And we saw a patient who might be appropriate for occupational therapy really soon. And, you know, communicating with the nurses, like, hey, like, we’d love to get in here early in seeing this patient as they’re coming out of sedation. And at the time, the patient was still pretty sedate. So they weren’t appropriate on that day. But we came back the next day and check back in the nurse said, “Hey, we’re leaving all sedation right now.” And we were like, “Oh, my gosh, we need an order.”
So we branch to the NP and we asked the NP for the order. And if we hadn’t asked the NP for the order, we probably would have ended up seeing that patient two to three days later. And the research says two to three days into the ICU when the patient is awake is when her at most most risk for delirium and developing delirium. So just even like the ability to get into the patient’s room earlier, is something that we’re doing. And it takes a lot of communication with nursing staff. Because if a patient’s really sedated, they’re not going to really see a need for an order at the time, but kind of like jumping the gun. And so we ended up going into the patient’s room and working with them as they’re weaned off of propofol and presser docks and everything. It was a lot of like coping and anxiety management, and reorientation and everything.
And the thing that I feel like was really a win for us is when we were back and we were charting and, you know, writing a note about the session, and the nurse came up to us and said, Hey, thank you for working with the patient. There’s no good way for someone to come out of sedation. And I just felt like that was a huge win for ot to build that relationship with the nurse. And the trust that they saw. Like we can be in there early and this is safe. And this is feasible, and we were actually able to help the patient out right so I just feel like the communication is so important and it could always be or improved.
Kali Dayton 20:02
And it’s so exciting for me to hear about how empowered you are, even as an OT student, you are empowered to advocate for patients. I think the same thing with physical, even speech therapy, you’re kind of dependent on the rest of your team as to whether or not you work with patients. And because it is that way, it’s created this culture of silencing you, you know, there’s not, there’s not this platform saying, You tell us if this patient is appropriate for occupational therapy, it’s been we’ll wait until the MP or the MD deems a patient appropriate for occupational therapy. And yet, they’re not always trained on what you bring to the table.
So how do they know when and how to apply you. So I love that you’re going to each patient, and making sure you’re not letting patients fall through the cracks. And then you’re open that communication and people are seeing what you’re doing and becoming receptive and learn about what you offer and provide for patients. That is so powerful, and I hope physical therapists do that as well. Yeah. And if a patient is deeply sedated, I think OT and PT have every right to ask about sedation. I know sometimes that can become very territorial. But in the end, we’re all here for the patient. Right? We all say we all yes. If we all understand why sedation should be minimized, then there shouldn’t be hostility when the question is asked, Why is this patient on sedation?
What is the indicator for sedation? And their answer is mechanical ventilation. I think it’s okay to open that conversation up further saying is mechanical ventilation, an automatic indicator for sedation, we would love to help the patient come off of sedation, we’re here to help you through that. Because every nurse knows, it’s not easy. And that’s why they stay on sedation for so long. It is hard when they come out of sedation, but you were there with all these tools, expertise and excitement, to help them come back to reality and be comfortable, whereas the nurses aren’t always trained on that they’re not comfortable. And they don’t have time.
Mallory, OT Student 22:04
Yeah, definitely.
Rachel, OT 22:06
And a lot of times to their answer is agitation as the other reason for not coming off of sedation. And I feel like that’s something that we can maybe help with, like Mallory started to kind of get to the bottom of their agitation and then help with that further.
Kali Dayton 22:20
I’m thinking about too, a few episodes ago, the episodes called sedated because she’s intubated and intubated, because she’s sedated. It’s dangerous. And it’s it’s happening, it happens so easily. Because if we address agitation with sedation, we just keep them on the cycle. And I’m thinking to this patient, she had been intubated because they’re trying to protect her airway. And because she had swelling in her airway, but that swelling probably went down long before she was excavated. Because when they were trying to wean down sedation, she’d come out agitated, and they say, “Oh, she’s not ready yet and resumed sedation.”
But if you had been there, as the expert on delirium as an advocate, to say, Oh, just hold the sedation, we’ll help her work through this. We’ll get her calm down, and we can just get this to about that could have saved her. So much suffering delirium, her PTSD would have been better, she would have lost so much muscle has this terrible rehabilitation. Like all those domino effects, you could have just dived in there and stopped falling volume of Domino’s, right? Yeah. And so I just love the thought of OTs being empowered to say we are experts on this, we do need to work with this patient. We are here as part of the ICU team and in a tactful collaborative way. Right? every right to be firm. Yeah, I love it. And so how will you work with the rest of the ICU team? Like what is your relationship with our OT’s?
Mallory, OT Student 23:45
That’s a really good question. I’ve definitely seen the dynamic between OT and RT as being really important and more important than I thought it was prior to coming into the ICU for the first time. I think, like I said before, my mentor does a really good job advocating for OT and asking those hard questions. So a lot of the times we’ll spend time talking with RT about the patient’s current status. And if they’re on if they have a tracheostomy if they’ve been on trach color before, why are they on tray collar right now?
What have they been capped before? And we love to, you know, ask those questions, especially if we can get a patient cap during an OT session that we were able to work on communication and coping and really allowing that patient to have a voice even if it’s just for like, 10 minutes, and we’ve had sessions where we’ve asked and you know, it’s gone really well. And we’ve had other sessions where no, we asked, and they they put the cap on and you know, maybe the patient just isn’t ready today and we weren’t able to work through the anxiety that came along with capping, but at least we tried. Right. So we’ve had Yeah, really dynamic and really, I think a really good good relationship with the respiratory therapists at our facility and like their support occupational therapy really well.
Kali Dayton 24:59
I remember when I started the podcast, that’s when I really started watching occupational therapists. Because they were always present, but I just didn’t. I wasn’t always in the room while they worked with patients, I didn’t see what they did. I was super curious. I started noticing those OT and RT dynamics when they were taking patients like ot was walking patients to the shower room. And Artis pushing the ventilator. RT puts the extension tubing connecting to the ET tube and OT is showering the patient.
And that had been so normal before. But once I started to talk, talking with teams outside of that euphoric bubble, what a powerful role ot was playing, doing working with functional mobility, but also those activities daily living there helping patients brush their teeth put their socks on while they are intubated. Yeah. And, again, when you’re in that environment, where almost everyone’s awake and walking and moving, you just see humans doing human things.
But now I realize a lot of that was because OT recognized that those were skills for daily living that they needed to preserve, and preserve dignity and just things that I as a nurse, or nurse practitioner, I wouldn’t have thought about, yeah, let this patient shower herself, lets her that her watch her own hair while she’s intubated. That wouldn’t have crossed my mind. But occupational therapy, you see them as human, and you recognize how important that is to them in that moment, and later.
Mallory, OT Student 26:20
Yeah, and I think we maybe even see things that nursing staff doesn’t see just because we spend more time for extended periods of time talking with the patient, right? Like the nurse is so important because they’re at the bedside 24/7. But ot we might be in the patient’s room, like I said before an hour at a time communicating with them that whole time. And I’m just thinking back to another example of how we work with the interdisciplinary team is our role with speech therapy. So we had a patient who is requesting something to eat and drink, but they weren’t quite ready yet.
And we have requested a speech consults. So along with that speech consult, the patient was also able to get a passing you’re about for the first time. So it’s great that, you know, we were able to see that need and an advocate for speech to get a console as well, because we’re not all consulted at the same time. And, you know, who knows how long it would have taken that patient to get a speech therapy consult put in if we hadn’t had us. And if the patient hadn’t expressed their need to ask that they, you know, we’re ready to eat and drink and like wanting to drink. And so now the patient is having a voice of verbal auditory voice that we can hear and communicate with. And eventually, hopefully, soon, we’ll be getting a swallow though.
Kali Dayton 27:33
And I’m thinking about these terms, humanize the ICU that we’re using, and I’m realizing that is going to be impossible without enhanced utilization of rehab services. Because those are not things that the rest of the team is trained on. And that’s okay, that’s why you’re there. But there needs to be more awareness, know how to utilize you. And I just feel like this direction we’re headed and maybe you know, team leads, like medical directors need to kind of steer the team. But you guys are the engine, you guys are like pushing up the gas saying, we’re going to be going this direction. Here we go. Here’s what we’re gonna do you have a leadership role in this? And how can we help occupational therapists recognize their ability to lead this out? And to really influence this?
Mallory, OT Student 28:18
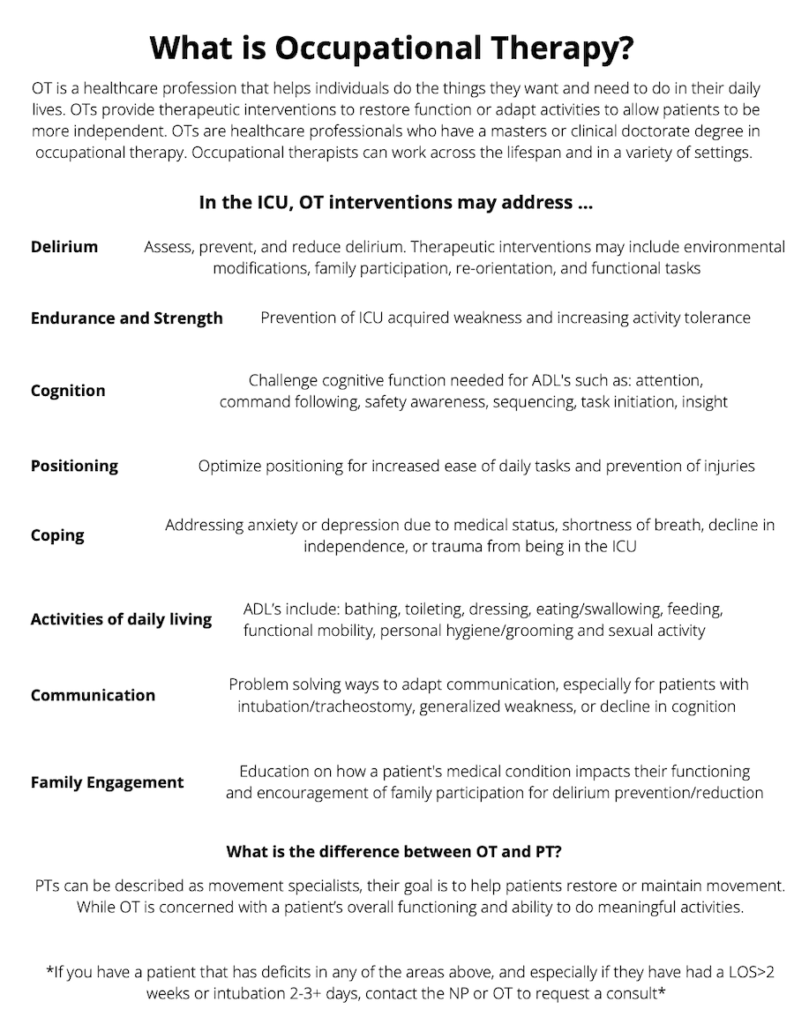
Yeah, oh, that’s a really good question. I feel like I’ve always had a very, like, quiet personality. But this is something that I’m very, very passionate about. And I feel like this is an area that I’ve really found my voice in and really just want people to know what occupational therapy is in the ICU and the ability that we have to see patients, you know, like you said before, as a person and to address their delirium, and to get in there early. And, and so as part of my capstone project, I’m creating a education resource for the nursing staff that’s going to be oriented to the floor.
And I believe it’s going to be sent out to all the nursing staff in the cardiovascular ICU. And it’s just a quick overview of everything that occupational therapists can do in the ICU, because, like I said, Before, the nurses at the bedside 24/7. So they see things that we don’t see, and they see needs that we don’t see because we’re not there. So if they know the full extent of what OT is, and I think we, you know, like we were talking about be able to better utilize our services. And as OT, we need to be able to advocate for ourself and be okay with people not knowing what we are and sharing, you know, our knowledge and our role with them, because no one else is going to do it for us.
Rachel, OT 29:30
And I think as far as placing consults for ot goes, I think the misconception is sometimes if someone’s arrest of zero and Cam negative, then they’re ready for therapy. Whereas it’s kind of the opposite for us. I feel like we can maybe help them most. If they’re cam positives, and the rest is something other than zero. So we can address some of those delirium components.
Kali Dayton 29:55
Absolutely. I noticed when COVID was hitting, we’re having more float nurses come in, you know, we’re Having more integration of different cultures, physical therapy came to me one day and said, I’m so confused. I had, you know, a nurse that I don’t know, stop me at the doorway and say no, there are two computers today, they can’t do physical therapy. And her jaw was just dropped. She’s like, that’s why I’m there. I am there for the delirium. I am part of the delirium SWAT team.
So I think, yes, we have that role understood. And he would just, I think we need to have better education about what delirium is how to treat it, all of that, then we plug in OT and say, here’s where they fit. And here’s why you should have a consultation from us every patient in the ICU, and I just think you can have big influence on sedation man sedation practices and caring for the ABCDE F bundle. Do you have thoughts on that bundle and message to the ICU community about that?
Mallory, OT Student 30:51
Yes, we have a lot of thoughts on the bundle. So people, people sometimes tend to lump occupational therapy into the E portion of the bundle, right? Early mobility, they think occupational therapy is a rehab service. So we’re going to put them in with the E, but actually, ot really has a strong presence in the D for delirium, right. So we do tap into early mobility just a little bit. But we really want people to know us as healthcare professionals who are able to address the delirium, right.
So, and we have other areas that we address too, like family participation, we love to involve family members, especially in the ICU, and with communication and coping and everything. And we also have the ability to assess and help manage patients pain, with non pharmacological methods, but what we really want people to know is that we have a role in the delirium part of the HF bundle.
Kali Dayton 31:48
Absolutely. And that should get you in there much sooner, you make the biggest impact. And I’m totally sold. And you guys work in a culture in which you are being well utilized. And you’re expanding that role through your advocacy. But what are some barriers within your profession and within the ICU communities, to being able to expand the occupational therapy role to its fullest
Rachel, OT 32:13
Barriers? I think probably would just be the lack of knowledge of what we can provide really, is the biggest thing. So we’re really working towards, you know, increasing everyone’s awareness, like what’s Mallory’s project here? So hopefully, you know, there will be more to come in the future?
Mallory, OT Student 32:30
Yeah. And I think even like on a systemic level, to like taking it back to the education that we receive, like, I’m kind of wondering, like, what kind of education do nurses or physicians receive on occupational therapy when they’re in school is it these are the rehab professions, ot PT, and speech, but that doesn’t really tell you what ot does. And then so it’s, you know, it’s not a health professionals foe, if they don’t know what OT is like, we have to be able to advocate for ourselves.
And it’s going to be a barrier that I think that we’re going to face in our profession for a long period of time, because people genuinely just don’t know, our full, you know, the full extent to what we can do. So whether it’s education on the level of you know, we’re in the ICU, talking to staff, but also just, I would love to see more education, occupational therapy for healthcare professionals who are still receiving your schooling.
Kali Dayton 33:18
I think you’re totally right, yep, we need to be teaching the interdisciplinary approach in school to have that expectation so that we don’t come out expecting to work in silos. And sticking to our own discipline, the research is so compelling as far as the impact that you can make, even mortality, length of stay readmission rates, if the rest of the ICU team knew how potent your treatments were, and changing outcomes, they would be really excited to utilize you at every possible moment. Any last shout outs for the ICU community?
Mallory, OT Student 33:51
Oh, man, yes, I have two, I have to call to actions. So if you’re listening to this podcast in, you are not an occupational therapist, but you work in critical care, I would definitely encourage you to find the occupational therapist who’s on your floor, and just reach out to them and start that conversation so you can better understand what they do. And they can better understand what your role is in interdisciplinary team.
And then if you are a critical care occupational therapist listening to this podcast, and you don’t currently address delirium in your practice, I would encourage you to dig into the research that’s out there. There’s a lot of really good information out there that supports occupational therapies role in delirium management. And I would also just encourage you to be an advocate for yourself and an advocate for your patients, right. So encourage you to have a strong voice and represent occupational therapy. Well,
Rachel, OT 34:44
just taking that extra step sometimes and having that conversation with whomever it is, whether it’s a nurse or respiratory therapists, to just let them know what we do, you know, just an extra minute of your time out of your day can just help with that whole progression. of increasing the knowledge of what we can do.
Kali Dayton 35:03
Absolutely, I think we all share the same vision for the future of critical care medicine. But we’re not there yet. It’s not standardized yet. But here we are now. And I see you guys being the ones chiseling away at the future. You’re opening the doors, busting down the barriers for future future occupational therapists, and I’m so grateful for everything that you’re doing the Mallory, you’re like busting into your profession with guns blazing.
I, I deeply believe nurses, OTs pts. I think as you start opening these doors, they’re going to come in and just step into their power and be empowered to practice at the top of their license and make the impact that they got their masters and doctorates to make. And yeah, I want OTS to know that they should have no hesitation in approaching anyone on the team. RNs, MDS, and NPS pas, to say, Can we get an order because I need to be in there and explain why there should be no hesitation.
And again, discussing sedation A to F bundle. Everyone should have a right to bring the evidence to the table, this hierarchy of the ICU needs to go and you’re going to be a huge part in changing the future. And now, do you mind if we include your memo that you’re sending out to everyone in the blog? Can we include that? Oh, yeah, we will part of the memo. The educational thing that you’re sending? Oh, yeah. For the nursing stuff. Yeah.
Oh, that packet that you’re sending to nursing staff was wonderful. I can email that to you. A perfect well, I’ll have it on the blog, as well as other studies related to occupational therapy demonstrating the life saving and cost saving the impact that you make on the ICU team. Thank you so much for all you do. Referring back to the powerful testimonial at the beginning of the episode, I just believe occupational therapies do and can save lives. So thank you so much.
Transcribed by https://otter.ai
References
Álvarez, E. A., Garrido, M. A., Tobar, E. A., Prieto, S. A., Vergara, S. O., Briceño, C. D., & González, F. J. (2017). Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: a pilot randomized clinical trial. Journal of Critical Care, 37, 85–90.
Brummel, N. E., Girard, T. D., Ely, E. W., Pandharipande, P. P., Morandi, A., Hughes, C. G., … & Jackson, J. C. (2014). Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the Activity and Cognitive Therapy in ICU (ACT-ICU) trial. Intensive care medicine, 40(3), 370–379.
Jackson, J. C., Pandharipande, P. P., Girard, T. D., Brummel, N. E., Thompson, J. L., Hughes, C. G., … & Ely, E. W. (2014). Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. The lancet Respiratory medicine, 2(5), 369–379.
Krewulak, K. D., Stelfox, H. T., Leigh, J. P., Ely, E. W., & Fiest, K. M. (2018). Incidence and prevalence of delirium subtypes in an adult ICU: a systematic review and meta-analysis. Critical care medicine, 46(12), 2029–2035.
Moon, K. J., & Lee, S. M. (2015). The effects of a tailored intensive care unit delirium prevention protocol: A randomized controlled trial. International journal of nursing studies, 52(9), 1423–1432.
Needham, D. M., Korupolu, R., Zanni, J. M., Pradhan, P., Colantuoni, E., Palmer, J. B., … & Fan, E. (2010). Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Archives of physical medicine and rehabilitation, 91(4), 536–542.
Rogers, A. T., Bai, G., Lavin, R. A., & Anderson, G. F. (2017). Higher hospital spending on occupational therapy is associated with lower readmission rates. Medical Care Research and Review, 74(6), 668–686.
Schweickert, W. D., Pohlman, M. C., Pohlman, A. S., Nigos, C., Pawlik, A. J., Esbrook, C. L., … & Kress, J. P. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. The Lancet, 373(9678), 1874–1882.
SUBSCRIBE TO THE PODCAST



 I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.
I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.