SUBSCRIBE TO THE PODCAST
Ventilator-Associated Pneumonia has significant lethal and financial repercussions for patients and our healthcare system. So why aren’t we panicking about it? Are hospitals really liable for the costs incurred from this ventilator-associated condition? Dr. Benjamin Wang, MD joins us to share the backstory behind VAPs in our US healthcare system and government.
Episode Transcription
Kali Dayton 0:36
Last episode we talked about the financial burden of continuous sedation and immobility in the ICU. The next two episodes, I want to narrow in on ventilator associated pneumonia as one of the big lethal and expensive dominoes of sedation and mobility. The average financial cost of ventilator associated pneumonia is $45,609. And the cost of life and quality of life to the patient, as well as increased burden on the ICU teams is incredible, yet difficult to measure.
So why aren’t we more panicked about it? Why do we have strict protocols for Foley and central-line care? But we have subjective parameters for oral care? Yes, our head of the beds are usually at 30 degrees. But no one is saying, “Wait, guys, if we sedate this patient, then we take away their ability to to cough, mobilize and clear their secretions and increase their time on the ventilator which will set them up to have ventilator associated pneumonia that could kill them.”
Stranger yet, when VAPs significantly increased health care costs. Why aren’t hospitals proactive about supporting the process of care that will prevent them? Why don’t they seem to care about the rates and risks of VIPs. Today, we have Dr. Benjamin weighing with us to provide the backstory behind ventilator associated pneumonia, and our hospital systems, and even the American government. Dr. Wang, thanks for coming on the podcast. Do you mind introducing yourself?
Dr. Benjamin Wang 2:09
Hi. Absolutely. Thank you, Kaylee. My name is Dr. Benjamin Wang. And I am a medical doctor by training. And I am as like like Kaylee here I’m very passionate about taking care of patients who are on mechanical ventilation.
Kali Dayton 2:27
And what is your nice your little expert? Not little, it’s big expertise. What are you specifically engrossed in right now?
Dr. Benjamin Wang 2:36
Well, I am not clinical, a practicing clinically, but I run my day to day is basically running a small medical device company called me that. And what we do at nev app is we create airway management, medical devices that get people off mechanical ventilation sooner by preventing infections and complications.
Kali Dayton 3:00
And what inspired you to develop this new endotracheal tube with infection and all of these things.
Dr. Benjamin Wang 3:06
So about 10 years ago, I was in the ICU. And as a I was a young doctor, and I was taking care of a young lady who had just given birth, but after giving birth, she had some excess bleeding ended up in the ICU unstable. And we had to put on a ventilator. Now at the time I thought if we do everything, by the by what we already know, if we do the right settings, and we apply the right drugs, then you know and otherwise healthy young 19 year old should do fine and and get off the ventilator and go home and, you know, be within your family.
But that wasn’t the case. And I got to see firsthand what happens when patients are basically ventilated for extended periods of time, my patient ended up catching a secondary infectious pneumonia due to her mechanical ventilation. And it was something that we really struggled to treat effectively. And unfortunately, that person, that patient died from that complication.
And at that point in my career, I was I was looking at the literature carefully and I was figuring out that when we put people on ventilators, their risk of getting a pneumonia is exceedingly high, too high in my opinion, and that as somebody needed to go into change that dynamic, otherwise patients would actually continue to suffer. So that was that was almost a decade ago. And that’s that’s what I’ve been working on ever since.
Kali Dayton 4:46
That is so tragic. And yet not that uncommon,
Dr. Benjamin Wang 4:50
not at all.
Kali Dayton 4:52
So, I guess let’s let’s back up and let’s zoom out. What is the definition of a ventilator associated pneumonia and what causes it.
Dr. Benjamin Wang 5:02
So, a ventilator associated pneumonia is a hospital acquired infection that occurs after 48 hours of a patient being invasively, mechanically ventilated, which is to say, we put them on a ventilator. But we also put either a tracheostomy tube or endotracheal tube or a plastic tube that either goes through the mouth into the lungs or through the neck into the lungs. And in order to qualify as a ventilator associated pneumonia have to have some proof, you have to have some positive cultures, or you have to have a positive x ray, you have to have some symptoms like a fever, or you know, high white blood cell count that kind of stuff, you have to have some proof.
But many times, it’s not very consistent, because not everybody will develop a fever, older patients tend to be cooler in temperature, and many times they don’t reach that threshold. At the same time, you know, patients who are immunocompromised may never present with a white count their white blood cell count just never gets that high, or you just may never be able to collect a proper sample that gives you a positive result.
And so many times, even though we have a fairly clear definition of what the pneumonia is, we don’t know if the criteria we’re using is actually very good at catching them. In fact, we know for a fact they are but they actually aren’t very good. So while the definition is kind of clear, the criteria are are inconsistent and unreliable.
Kali Dayton 6:45
Who sets the criteria? Is this something standardized in our community? Or does it depend per system? Or how does that criteria evolve?
Dr. Benjamin Wang 6:54
Well, this is the bad news, we I mean, it was kind of just grandfathered in, over the years that we assumed pneumonia should look like this. So it was basically based on committees of recommendations, but not really a lot of scientific proof. The tragedy of all this situation is that we’ve actually moved away from the definition and found the other definitions that are a lot less reliable, and remove the surveillance requirements.
So let me let me back up and tell you what is been happening in our critical care and infectious disease community surrounding this problem. So before 2009, there was actually about a decade of research focused specifically on ventilator associated pneumonia diagnosis. And and we knew that the definition was clinically subjective. It was poorly defined, and it was not often reported, inconsistently at best.
So the powers that would be at the Center for Medicare and Medicaid service saw this problem knew that it was an clinically significant, and they began penalizing hospitals based on the number of cases they reported. That was in 2009. So because there weren’t any good solutions, you know, and solutions that address people on Medicare, mechanical ventilation are often expensive and difficult. Hospitals, this basically got together and they basically said, you know, the strategy should be we would report less of these cases, because if you report less, then you don’t get penalized. And so then the number of cases reported cases of ventilator associated pneumonia in this country fell over 80%. After that, after that regulation came in place.
Kali Dayton 9:04
So the cases probably didn’t change. The reporting changed.
Dr. Benjamin Wang 9:10
Exactly. Actually, in 2016. We had a big report on something like 25,000 patients from from the basically from Medicare, and they basically proved that the rate of ventilator associated pneumonia did not change. What happened was the reporting changed, and the rates stayed the same, which means patient had no improvement in terms of their outcomes. And we just decided to sweep them under the street this problem under the rug now.
It’s not to say that the powers were be didn’t know they have a problem had a problem. Well, in 2014, the CDC actually came in and revised the definition of ventilator associated pneumonia, knowing that they had a surveillance problem What they did is they said, Well, if somebody has worsening ventilation, basically ventilator settings, they said, if they were doing worse, because of mechanical ventilation, then the results should show up on the settings we use on the ventilator.
This is all in theory, there was no data to support this, this new definition, which we call ventilator associated events, and they basically made it a definition to try and catch ventilator associated pneumonia.
Kali Dayton 10:37
So you could have a patient going into septic shock,
Dr. Benjamin Wang 10:40
and their ventilator settings could stay the same. Oh, my gosh. And then the hospital wouldn’t have to report it. Now, the funniest thing is other countries saw what we were doing. And we’re asking around and trying to do research to figure out if we had hit on something important if somehow we had figured out a real good way of surveying ventilator associated pneumonia, improving outcomes, so they did their own studies and use our definitions.
Kali Dayton 11:10
This is embarrassing.
Dr. Benjamin Wang 11:12
I mean, it’s it’s it’s good that the scientific community is doing this because otherwise we wouldn’t know whether it’s working or not. Well, absolutely. Researchers in the UK and France basically did the research based on the data they were collecting. And they found out that our definition was catching less than 15% of the ventilator social modal, which means the death, the new definition for ventilator associated events, was trying to catch everything and was actually missing the thing it was designed to, to basically address, which was any reality, the reporting problem around ventilator associated pneumonia.
And it’s so funny because this is a perfect example of that we we had a problem we were doing not so well at it. And then, you know, regulators stepped in and made the problem worse. Not only for patients, but for hospitals and, and even their own agency. So back in 2019, recognizing that they had made a mistake that there was a problem with the surveillance criteria, they remove the surveillance requirement altogether. So now hospitals, even though many of them still do this, internally, they don’t have any reporting requirements or surveillance requirements for ventilator associated events, even.
Kali Dayton 12:41
So there’s still the penalisation of it right there. So it’s not going to cost them money to do the right thing to report the harm that’s actually occurring.
Dr. Benjamin Wang 12:51
Just to clarify, they lose money, even if they don’t report it. Because when a patient does, does poorly in the hospital, they don’t get paid more, they’re just not incurring the end of the year penalties. But when a patient doesn’t do well, the hospital still have to pay for the additional care. So even without the penalty, they are penalizing themselves.
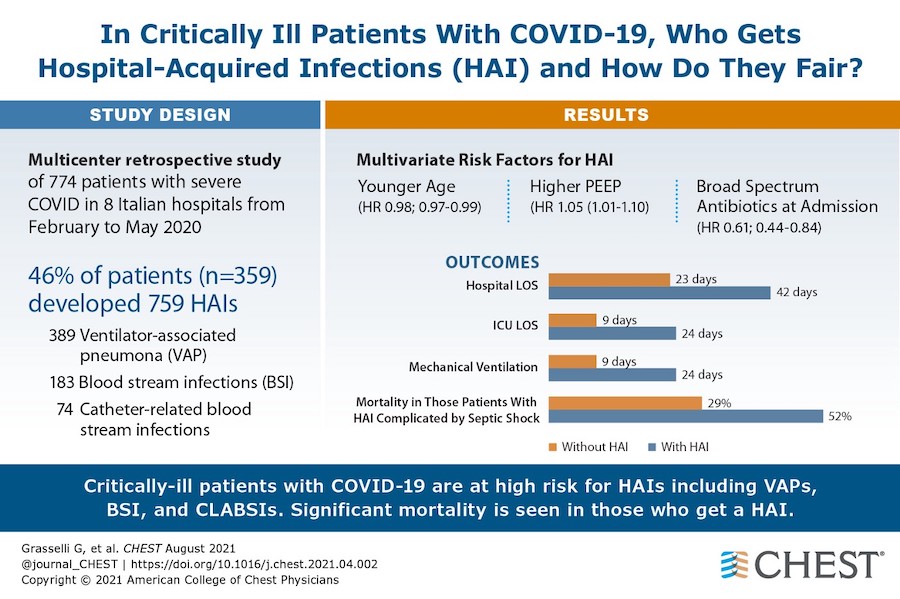
But what’s also happening is during a pandemic, when there are so many patients who are mechanically ventilated, you can imagine if a large percentage of the patients that are put on a ventilator don’t get off the ventilator soon or in a healthy manner. It puts an extreme amount of burden on our healthcare system. And that’s basically what we’ve been struggling with.
During the pandemic. It’s not, it’s not that we that community acquired cases and community, you know, people sick at home is a huge problem for our healthcare system. The real problem is when people get hospitalized and we don’t have enough beds and equipment and supplies.
Kali Dayton 14:00
And then if we do have an in a bed, when we do have them on a ventilator, we have this system that sets them up to spend days, two weeks, two months longer, occupying those resources that we need. This has resonated so much with what I’ve been experiencing, even talking with families of ICU member patients, looking online, ICU support groups, COVID-19 support groups.
Across the board, almost every single person is saying, basically my mom was doing better and then she started to have higher white blood count or her ventilators hadn’t spent backup. And they’re looking for sources of infection. Yes, I’m like, Let me guess let me guess, because they’ve been immobilized, sedated Lane supine in bed or grounded this whole time. So yet, if you talk to hospital systems, and you say, I can help decrease your ventilator associated pneumonia rate, what do they say?
Dr. Benjamin Wang 14:54
They say “no, we don’t have that problem. We’re we’re good hospital and we take with already taking care of that completely.” And the data is so stark because our European counterparts during the pandemic are reporting rates of ventilator associated pneumonia in these COVID patients that are astronomical. They’re 40-50% of all ventilated patients.
Kali Dayton 15:23
And what have we been reporting?
Dr. Benjamin Wang 15:25
We haven’t been reporting. That’s right. So we don’t even we don’t even know when I approached some hospitals, they’re still in the denial mode. And they basically say we have zero. And statistically speaking, the only way you have zero pneumonia, secondary pneumonia in these cases is if you have no patients, and it’s literally impossible to have none of these infections at this point.
Kali Dayton 15:54
And mortality rate for ventilator associated pneumonia?
Dr. Benjamin Wang 15:59
Is an increased…… oh, what we know from our European counterparts is it increases mortality, something between 15 and 25%. And that’s, that’s, that’s already compared to patients where we don’t know if they have a pneumonia and they end up dying in the hospital. So it’s not a good, the data points aren’t very good. And because the patients are already very sick, we don’t know exactly. If we’re missing some of the pneumonias, and patients are dying from it.
Or if we’re catching more of them. pneumonias and finding that you know they’re doing a little they’re not doing as bad. But what we do know is that when you and it’s it’s pretty common sense if you’re sick with a viral pneumonia, and you get another second pneumonia happening at the same time, it’s usually not good for the patient, I can say almost certainly it’s not good for anybody.
Kali Dayton 16:54
You’re already has a compromised body that’s gone through so much. Especially if they’ve been sedated and mobilize they’re so weak. And a lot of times I’m seeing in these cases that they’re nearing the end of the COVID pneumonia like their ventilator settings are decreasing there, if not minimal, they’re trying to liberate them from the ventilator and then bam, yep, now this new infection has caught up with them.
And they don’t have the reserves to fight it like they did with a COVID pneumonia, they don’t have this year strength there, the app, the atrophy is so profound delirium is already there. Right? They already have injured other organs. And now we’ve introduced a whole new infection for them to fight and it is lethal.
Dr. Benjamin Wang 17:37
And just to clarify, I mean, I want I want to take a step back even from that and say, say this, we’re putting an enormous amount of stress on the body and the patients. And we know from the literature, that these pneumonias are time dependent, which means the longer a person spends on a ventilator, their risk of pneumonia goes up their outcomes go go the other way.
And so the strategy should be to look carefully at what we are doing to these patients to get them off mechanical ventilation sooner. And to make sure that while they’re on mechanical ventilation, remember, this is probably the most vulnerable time in a person’s life when they’re completely sedated. They’re paralyzed. They don’t they’re not breathing for themselves. And they can’t even communicate a cough or anything to prevent bad things from happening to them. So it’s not surprising that if you can adopt strategies to reduce the time a person spends in that state that the outcomes ultimately become better.
Kali Dayton 18:52
And we’re absolutely going to get deep into the strategies, the solutions. Next episode. What are some of the main causes or risk factors in addition to prolonged time the ventilator? What else can cause ventilator associated pneumonia?
Dr. Benjamin Wang 19:05
Well, the risk factors are actually identical to some of the risk factors that we’ve seen for COVID patients that don’t do well. It’s time on mechanical ventilation. It’s the use of a invasive mechanical ventilation, which is, you know, if you put something in a patient for a long period of time, it tends to get dirty being being very heavy, having comorbidities like diabetes or being immunosuppressed and basically having other things that push down your immune system and immobilize you just the fact of being paralyzed is a risk for ventilator associated pneumonia and extended and poor outcomes in general.
Kali Dayton 19:52
Throughout my seven years in the wake and walk in ICU, I really think I saw two ventilator associated pneumonia that I can remember and And because that team really has to defend their practices, they scrupulously check their outcomes, self excavations, falls, ventilator associated pneumonia as they are scouring their outcomes, they have a nurse dedicated to watching those reports, and making sure we keep track of them so that we know how effective we’ve been. So this is a team that really cares about these things. And I would hope that the hospital system that they’re a part of reports them sounds like it’s up to the hospital system, not necessarily the team.
Dr. Benjamin Wang 20:28
It is really is, because what will happen is, even when the team finds one and documents, it’s still up to somebody else that is unrelated, oftentimes, the clinical team to report the cases.
Kali Dayton 20:42
Oh, that’s sketchy.
Dr. Benjamin Wang 20:45
So while you may, if you were to do a chart review, you find you’d find ventilator associated pneumonia. And you’d find reports in the department that they’re improving, you know, in their measures and their quality improvements, bots, somehow that information doesn’t get reported sometimes doesn’t make it up to survey, you know, doesn’t make it up to other types of reporting. And it can be due to a number of different factors that could be by design, basically.
Kali Dayton 21:17
So it may or may not be just one person or one little entity, that’s
Dr. Benjamin Wang 21:22
Kali, you know, new, you know, as well as I do that healthcare is complicated. The more hands on, the more people involve the more chances that things can go wrong, or they can go a different direction.
Kali Dayton 21:36
And it’s easy to hide these kinds of systemic errors.
Dr. Benjamin Wang 21:40
There is no federal regulator that comes into the hospital and says, I want to do a chart review. There is no,
Kali Dayton 21:46
and yet they’re caring about whether or not our coffee is covered at the nursing desk. Oh, no, it wasn’t not worth adding to the mortality of patients.
Dr. Benjamin Wang 21:54
The accountability in some of these places is quite different. And so that’s, that’s one of the challenges we have in healthcare. Well, these
Kali Dayton 22:02
Two cases that I’ve seen a ventilator associated pneumonia that I can think of and recall right now, they were both sedated and immobilized. One was a young man that had tumors all throughout his trachea, and he had like a deal wired into tracheal tube, and his airway was fragile. So we did stay at him. And he got MRSA pneumonia.
Dr. Benjamin Wang 22:22
Yep.
Kali Dayton 22:23
And it was traumatizing for us. And I think, if I remember correctly, they may that may have led to his demise. Yep. Granted, he was. Prognosis but But nonetheless, it was that was the last straw. And that was such a new concept, because that team is not used to seeing that because patients are awake, moving coughing, they’re not getting the same stuff for subglottic aspiration.
And it’s just not that common to have patients having ventilator associated pneumonia, if I can remember to distinctly it’s because that was a big deal. And we all were aware of it, we talked about it. It was almost like a case, I’d have to say this is why we treat patients the way we do as a standard because this is what happens when we don’t. And we’d never want this to become normal. But our teams really recognizing I mean, they may charter document it, but are they saying hey, this could have been preventable? This is a big deal. This is a I know, we talked about collapses and UTIs and things like that, but that, are they talking about it,
Dr. Benjamin Wang 23:19
They really aren’t many times and to be quite. I mean, there aren’t a lot of colleagues that end up causing death and end up hospital, you know, causing patients to end up on a ventilator for longer periods of time. So the consequences of certain infections are quite different. It’s not to say that we aren’t that these infections aren’t important, they really are important. I mean, all infections are really important for for patients.
The the end result, though, I would imagine should also take should also be taken into account in these cases, because these conventions do cause death. And quite frankly, we don’t do a good job of diagnosing these infections in general. While you may have only seen two cases of diagnosed ventilator associated pneumonia, it is very likely that you’ve seen hundreds of cases of Pseudomonas Klebsiella pneumonia MRSA pneumonia and what has happened in these cases is we know from the literature that the bacteria and the fungal infections that are involved in ventilator associated pneumonia are quite different than what we see in the community.
But what happens is when you come into the hospital, there is no incentive to report it as a ventilator associated pneumonia, there’s actually a lot of disincentives. So what will happen is, many of the doctors will look at this and say, Well, this was somebody will say, Well, this was a community acquired pneumonia. And that simply wasn’t true because we just don’t see Klebsiella Pseudomonas actinic factor….. these very rare types of pneumonias in the community in high numbers, maybe sometimes once in a blue moon in immunocompromised patients. But I suspect of you, if one were to look closely at the antibiotic use, and the bacteria and the funguses involved in these infections, you quickly find out that there was a lot of ventilator associated pneumonia that was never reported and never considered.
Kali Dayton 25:34
And how do they, how do they get around if they’ve done a culture on admission, and then two weeks later, you do another culture and it grows completely different things.
Dr. Benjamin Wang 25:43
Remember, the doctors know that when they report something as an infection, they, they can simply report it as a pneumonia of unknown origin or on you know, they don’t know where it was picked up. And they treat it doesn’t change the treatment plan, you still use antibiotics, and you still do, do you know, the same kind of kidney care and the same kind of heart consults and everything that you would, if it was, regardless of that diagnosis, once you diagnose somebody with pneumonia treatment plan is similar in many, many cases.
So if there’s no incentive to report it as a ventilator associated pneumonia, and there’s no training around, have letting them know that this is a problem. Many times the clinicians can basically look at this and say, well, Leah, you know, I see Pseudomonas pneumonia all the time, it’s not a problem, I’ll call it Pseudomonas pneumonia, not ventilator associated, or I call it community acquired, or I call it infection of unknown origin. And you can get away from really trying to figure out what what happened in the in the case of of diagnosing and ammonia. And what that does it, it further complicates the surveillance issue.
Kali Dayton 27:00
Interesting, because no one wants this harm to occur on their watch. Right? So there’s, I mean, even if they’re not going to have direct penalization, it’s kind of a, an ego thing or a pride thing to say, right? If we say that, that they got this while they were on the ventilator, and called a ventilator associated pneumonia, it doesn’t feel good, it doesn’t make us feel successful.
Dr. Benjamin Wang 27:22
Right? Right. But I mean, you know, just like the pandemic, it’s like we can do the things that make us feel good. Or we can do the things that make a difference. And, and doing the things that make a difference. Oftentimes, it’s not the easy way, the easy thing to do. But it’s really the right thing to do in the long run, because the more we try and sweep problems underneath the rug, and try to act like they don’t exist, what happens is they they come back to bite us in the butt.
Kali Dayton 27:55
Absolutely, I’m worried if you know, if hospital systems don’t recognize the systemic contributions to death, to hospitalization costs and those kinds of things, when you or I, or hopefully the teams themselves try to pitch this elevated process of care. Now, we can’t use this car to say we can do this process of care can decrease your ventilator associated pneumonia rates that we know are a problem. But they’re unaware that it’s a problem and they’re in denial. So then that discussion is thwarted.
Right? That should be part of our of the the cards that we’re playing to say, here are the rates of the delay social pneumonias that are caused by these risk factors. This is what we need to change. Here’s how we can improve patient outcomes and always possible. But if we’re in denial, we can’t address it, we can’t fix what we can’t confront.
Dr. Benjamin Wang 28:47
Right? Right. And if if there’s anything that the pandemic has taught us is that if we don’t confront it, it really comes back to be a bigger problem, rather than small, rather than a manageable problem. And denying that we have a problem is is not a good strategy going forward. I mean, what we’re talking about has real consequences, not just for patients today, and and for patients that have actually had these problems, but for future generations to antibiotics. And this type of care are the only medications that we have that get worse and less useful every time we use.
You know, you think about our our blood pressure medications, our blood pressure medications are going to work 50 years from now, 100 years from now, they’re always going to work, you know, well, hopefully we’ll get a couple better ones with less side effects and they’re more effective. Banana antibiotics, the antibiotics that we use today will rapidly become less effective in the next couple of years and If we don’t address infectious problems, such as this sooner, we may end up having as a world where our antibiotics don’t support modern medicine. And that’s really concerning too.
Kali Dayton 30:16
That’s a terrifying prospect. That’s really unsettling. And even from my side, just thinking about how we’ve suddenly, I mean, not suddenly, but over time throughout the pandemic normalized, the use of medazepam. First to first go to sedative, this generation isn’t even going to be aware of any alternative forms of treating patients is just standardized.
And now we can’t even talk about how harmful it is we don’t realize how many ventilators will shift ammonia medazepam, deep sedation immobility lead to, then we have less incentive to change. And this is going to just normalize this really bad practice and impact many generations of patients to come. And then we’re going to continue to have more needs for these antibiotics that are going to become less effective. That is terrifying.
Dr. Benjamin Wang 31:10
You know, and you know, I hear a lot on NPR and podcasts about memorializing the 800,000 or so victims from the, you know, victims from the pandemic in our country, I can think of no better memorial to those patients, and figuring out how to improve care for the people who need this type of care in the future. I really can’t, you know, if there’s one lasting legacy that we can impart on our healthcare system is, if we can improve care here, it makes a big difference.
Kali Dayton 31:50
Oh, that’s a that’s a beautiful thought. Interviewing survivors and family members, they are so eager to dedicate their suffering, attention of harm of others. And that really should be Yeah, one of our big motivators to not allow their deaths to go in vain make this the ultimate research. We have had the largest sample size in history of ventilator management.
And we do need to dissect it and be honest and real with ourselves about the good, the bad and the ugly, what worked, what didn’t work, and we need to decide who we’re going to be and what we’re going to do moving forward. Pandemic hopefully isn’t gonna last forever. But these practices cut. Yes, that’s the key. It’s time for accountability. Real talk. Next episode, we’ll get into the solutions moving forward. Anything else you would add to this discussion? Dr. Wing?
Dr. Benjamin Wang 32:46
No, I think we covered pretty well and and I hope your listeners enjoy what we’ve discussed. All
Kali Dayton 32:53
the studies, all the information you shared will be included on the blog. So go to your research. Thanks so much. If you want to join in on the conversation, leave a voicemail at 801-784-0472 or reach out to me on Twitter.
Transcribed by https://otter.ai
References
Early Mobility and ABCDEF Bundle prevent VAP:
Klompas, M., Anderson, D., Trick, W., Babcock, H., Kerlin, M. P., Li, L., Sinkowitz-Cochran, R., Ely, E. W., Jernigan, J., Magill, S., Lyles, R., O’Neil, C., Kitch, B. T., Arrington, E., Balas, M. C., Kleinman, K., Bruce, C., Lankiewicz, J., Murphy, M. V., E Cox, C., … CDC Prevention Epicenters (2015). The preventability of ventilator-associated events. The CDC Prevention Epicenters Wake Up and Breathe Collaborative. American journal of respiratory and critical care medicine, 191(3), 292–301. https://doi.org/10.1164/rccm.201407-1394OC
Zang, K., Chen, B., Wang, M., Chen, D., Hui, L., Guo, S., Ji, T., & Shang, F. (2020). The effect of early mobilization in critically ill patients: A meta-analysis. Nursing in critical care, 25(6), 360–367. https://doi.org/10.1111/nicc.12455
Improved Endotracheal Tube Technology:
Dr. Wang’s endotracheal tube technology- https://nevap.co
Dragoumanis, C. K., Vretzakis, G. I., Papaioannou, V. E., Didilis, V. N., Vogiatzaki, T. D., & Pneumatikos, I. A. (2007). Investigating the failure to aspirate subglottic secretions with the Evac endotracheal tube. Anesthesia and analgesia, 105(4), . https://doi.org/10.1213/01.ane.0000278155.19911.67
Mao, Z., Gao, L., Wang, G., Liu, C., Zhao, Y., Gu, W., Kang, H., & Zhou, F. (2016). Subglottic secretion suction for preventing ventilator-associated pneumonia: an updated meta-analysis and trial sequential analysis. Critical care (London, England), 20(1), 353. https://doi.org/10.1186/s13054-016-1527-7
SUBSCRIBE TO THE PODCAST