SUBSCRIBE TO THE PODCAST
What role do registered dietitians play in patient outcomes in the ICU? Why is malnutrition such an emergency? How can we better utilize the expertise of registered dietitians? What does the latest research show about our performance with nutrition in the ICU?
Megan Dockweiler, MS, RD, CNSC, and Amand Bakko, MS, RD CNSC share with us their expertise as ICU Registered Dietitians.
Episode Transcription
Kali Dayton 0:00
Okay, it’s way past time to talk about registered dieticians. It is a shame to have left out such a huge part of this ice puzzle. I have been learning so much throughout this podcast and I’m grateful to you amazing listeners that have reached out and said hey, Kaylee, you need to discuss this and include that. I love it. I am grateful for all of you. We discuss interdisciplinary collaboration in the ICU, not just to make sure everyone feels important than saying we are working through this because we have to understand the vitality of everyone’s role.
The gaps in our practices are almost always a result of the gaps in our knowledge. We cannot work together if we don’t understand the value of everyone’s roles, and how to best utilize each other’s expertise with that. Megan and Amanda expert ICU dieticians Join us now to open our eyes to the central role registered dietitians play in the ICU. Okay, Manda and Megan, thank you so much for coming on the podcast. I have been thrilled about this episode. We’ve been needing it for a long time. Would you mind introducing yourselves?
Amand Bakko, MS, RD CNSC 1:46
Yes, of course. Thank you for having us. We’re very excited. My name is Amanda. I’m registered dietitian. I did my undergraduate degree in Indiana. I then went on to complete my internship and my master’s degree in Illinois, where I then worked as a clinical dietitian for two years. And then I moved to Virginia where I’ve been working as a clinical dietitian still for the past year.
Megan Dockweiler, MS, RD, CNSC 2:10
And my name is Megan. I am also an Registered Dietitian. I completed my undergrad in Rhode Island went on to complete my master’s and internship also in Illinois. And then I moved back home to Long Island where I was working in Brooklyn, then moved to Virginia as well.
Kali Dayton 2:28
Awesome. And I think we crossed paths because I was on a ICU dietitian page, looking for collaboration. And I’m pretty sure I made a mistake. And when I post I think I said nutritionist or something like that, and I got massacred. So well, you clarify for all of us. So no one makes the same mistakes. Tell us about what registered dietitians are and what you do and your role on the ICU team.
Amand Bakko, MS, RD CNSC 2:56
Yeah, so nutritionist, some people use it synonymously dietitians love to be called dietitians, so a little bit of a difference. So we do have an undergraduate degree that we have to complete. The master’s degree is optional right now, by 2024, it will be required. So a lot of dietitians do hold that master’s degree, but it will be required soon after the education would go on to complete the 1200 hour internship. So it’s mainly clinical based depending on where you do it, but it kind of covers every area of dietetics. So it’s 1200 hours that is required to sit to take the national exam.
So then we take an exam become credentialed through the academy. And then we do have advanced certifications as well. So then we can go on to do nutrition support peds, weight management, oncology, renal. Some of those certifications require us to have a certain amount of hours in the field, some don’t it’s kind of It depends. Some of them, you have to take the exam every certain number of years depending on which one it is. So it is just wanting to keep up to date on the research, wanting to make sure that you know you’re fulfilling the competencies.
So the thing that is the difference between the nutritionist and the dietitian, we do medical nutrition therapy. So meaning that we are able to provide education to individuals with diabetes, kidney disease, those types of things specific to the disease state whereas nutritionist that is not allowed in some states is actually illegal because dietitians can be licensed in certain states.
Again, it’s not all states just kind of depends. So some require licensure, some states are credential, and some states don’t have anything at the moment. And so nutritionists like I said, can’t do the medical nutrition therapy but they do have to go through some training. It can be anywhere from like a six week course to a two week course two week course. Kind of depends. It can be you know, an undergrad degree, but it’s kind of just like an if statement of someone calls themselves a nutrition So we don’t exactly know where they’re getting that degree from.
Kali Dayton 5:03
Okay, so yeah, it’s kind of like CNA versus RN, or CNA versus NP like they’re very different education focus, credentials, capacity. So thank you for the specification. And so when it comes to your role on the ICU team, how do you approach caring and consulting on an ICU patient?
Amand Bakko, MS, RD CNSC 5:27
Yeah, so we just kind of wanted to point out just as a whole, we both work in the intensive care unit as, as well as just on the general floor. Dieticians as a whole we see the patient, you know, we’re not just looking in their chart briefly and seeing what’s out there on the then running upstairs, go see them. We look at everything medication Labs has medical history, we want to know, you know what disease states we need to address.
When we’re in the room with a patient. We look at micronutrient deficiencies, and we look at food drug interactions, we are heavily we have a heavy communication with the multidisciplinary teams in the hospital, we on a daily basis, we talk to the care managers, of course, the doctors, nurses, we work with speech really closely. So we work with a lot of the disciplines. And so when we’re seeing a patient in the ICU, the main thing is we you know, want to see how we can feed them. We want to see you know, if they’re in the ICU, whether they’re intubated or not, you know, one of the projects that we are working on is early enteral nutrition. So we want to make sure that we’re screening these patients as soon as they get into the ICU and figuring out if they’re on an oral diet, if they are NPO, if to feed as appropriate, parenteral nutrition as appropriate. So that’s kind of where we start up.
Kali Dayton 6:41
And I really appreciate that because you guys have a much broader perspective than many of us in the ICU because you see them after the ICU. You see what their recovery is like. And it sounds like that’s kind of what’s motivating you to be more proactive in the early stages. What is it like on your team? I know that some teams dieticians aren’t even really part of the discussion, some teams their integrated part of rounds. How was it from your team? And how should we be using dieticians?
Amand Bakko, MS, RD CNSC 7:13
Definitely, in rounds as much as possible, I think Megan and I both have the place where we’re at now and where we previously worked. We were included in rounds. Unfortunately, that’s not the case everywhere for dieticians, you know, it’s hard because a lot of times people don’t know what the dietician does, sometimes our office is stuck in the kitchen. So our office isn’t up on the floor, we’re not having those daily interactions with doctors, at least face to face.
So I think that, you know, getting our faces out there being up on the floor as much as possible, having those in person conversations with doctors, nurses, the multidisciplinary team pharmacists, that’s really the key role. Coming to the facility that I’m at now, I feel like we have a huge or better communication with multidisciplinary teams, everyone is just very open. So that’s really great. Everyone knows who the dieticians are, which isn’t always the case. So just getting getting our faces up there, because a lot of people just assume that we see patients, because they need a diet change, or they need their tray ordered. But that is you know, the kitchen. And that’s completely separate from what the dieticians do.
Kali Dayton 8:23
And it sounds like you guys have a lot more to offer than just changing it to a renal diet, you know, there’s so much more to it that I think we don’t appreciate,
Megan Dockweiler, MS, RD, CNSC 8:30
we screen our ICUs individually, like we can we do get consulted most of the times, but if we see that their BMI is under or we screen them previously for malnutrition, or things like that, like we can put ourselves onto the case during rounds, and we’ll discuss and then we pipe up like what are the dietitians have to say and then we can go on, or if we hear something during rounds, and then that we need to go see the patient, then that will make us trigger us and
Kali Dayton 8:59
we can Oh I love that. I hope that that’s part of everyone’s protocol is that you guys are able to say, hey, you need us on this
Amand Bakko, MS, RD CNSC 9:07
is very individualized per facility, I think we have a lot of leeway where we can kind of just bring ourselves onto the patient if we want to see them. I don’t think that’s always the case. Sometimes you do need a doctor’s order. And you know, if it’s not an ICU, the doctor isn’t always present. A lot of the times if the dietitian can’t find them, then it might be something that just takes a little bit more effort.
Megan Dockweiler, MS, RD, CNSC 9:28
And different states have different rules like I know back at in New York and my old hospital like they had some rules taken away. So they weren’t allowed to but previously when I worked in the stick you during rounds, we had the freedom whereas now they’re backtracking a little bit. So it does depend. Yeah. And
Kali Dayton 9:46
We’ll get into that later. But I’m that has to impact outcomes I’m thinking about a couple many episodes ago, I interviewed a CNA down in Arizona, who was watching on their COVID unit these patients on Hi Flint as a candidate Love breathing in the 40s they were not allowed to get out of bed and they didn’t have internal feet going. And I’m sure dieticians just cringe at that. So how much would those outcomes those patients, how many innovations would be avoided? If there were dietitians that were able to come in and stormed the palace, right?
And say, you’re missing a piece of the puzzle here. We’re here to bring it. So I would invite anyone that’s listening to really ask and question your own teams, what role are your dieticians playing or allowed to play? And how can we better utilize them? I am really excited about your role on your team, I think you guys have a lot of really cool things going. And you guys contacted me because you as dieticians, are pulling your team together to implement the ABCDE F bundle, which is exactly what a multi and interdisciplinary team should be about and should be allowed to do. Everyone should be able to pull team together to require or encourage evidence based practices. So how did that even start? How did you get to that point of ringing the bells in your own team.
Megan Dockweiler, MS, RD, CNSC 11:04
So we started listening to the podcast and wanting to initiate the process of combining all the disciplines together. Like I said, like Amanda said, we had already started the early enteral nutrition protocol trying to get patients fed. While we are not a part of the ABCDEF bundle, we just kind of wanted to push ourselves in there. And so we need to kind of like the ICU, multidisciplinary early interventions protocol, we have a new ICU tower being built currently, that’s under construction.
And so we went into our intensivist and said, Hey, this is what we want to do. What do you think, can we get everybody together and make this happen, basically, so we’ve had a couple of meetings so far, we have one every month to just get everybody together. It includes the intensivist, the ICU nurse manager, the ICU, clinical coordinator, the director of rehab, along with PT, OT, and SLP, various members, whoever wants to be involved with that. It it also involves pharmacy, and then two nurse champions that we picked that were very intrigued about the bundle and wanted to be a part of it.
Kali Dayton 12:11
Oh, that is so exciting. And what kind of feedback are you getting? Are these other disciplines eager to do this as well?
Megan Dockweiler, MS, RD, CNSC 12:19
Rehab had already started their own early mobility, but it wasn’t really a part of everybody, they had just started coming to rounds and everything. So they kind of put themselves on to the cases as well and get consulted. But it wasn’t really like the culture needs to change. So we had our own bundle, they had their own bundle. So we kind of just tried to get it all together.
Kali Dayton 12:44
Yeah, and you make a really good point. That N was the ADA F protocols, bundles, and nutrition isn’t always specified. But it really should be and I see some of our nutrition research coming and integrating into this big movement to focus on long term outcomes of ICU survivors. I think there is a movement to integrate nutrition, I think we’re realizing that early mobility is a struggle when patients are malnourished.
That part of early mobility and preserving muscle and function is nutrition, which you’re all shaking your head because that’s a done on the medical and sometimes nursing side. It’s not so obvious, especially when we have obese patients we make really inaccurate assumptions about their nutritional status. So why is it so important to be so aggressive and early with nutrition in the ICU?
Amand Bakko, MS, RD CNSC 13:37
I think the main thing is just the fact of the percentage of patients that come into the hospital already malnourished. I mean, some patients definitely get malnutrition in the hospital if it’s a prolonged hospital say. But you can probably just guess if a patient is coming in, especially to the ICU, their nutritional status is really low. So whether that be and that’s part of our assessment, we talk to patients, whether that be you know, we’ve had, they’ve had a poor appetite for a month, two months, they haven’t been eating anything, they’ve had significant weight loss.
So part of what the dietitians do, we identify and treat malnutrition in the hospital. So we’re using Academy of Nutrition and Dietetics and Aspen criteria to diagnose someone. And so that includes a weight history, the diet history, and we assess for muscle or fat loss. So we do touch our patients feel certain areas of their body to try to help support that diagnosis for malnutrition. And when someone is malnourished if we can identify that that’s when we want to get that aggressive nutrition started, whether it be enteral nutrition, or a PO diet. We want to try to get as soon as possible
Megan Dockweiler, MS, RD, CNSC 14:45
….and while malnutrition is under under diagnosed in the hospital, approximately like 1/3 of patients who are not malnutrition, malnourished on admission become malnourished throughout the admission.
Kali Dayton 14:58
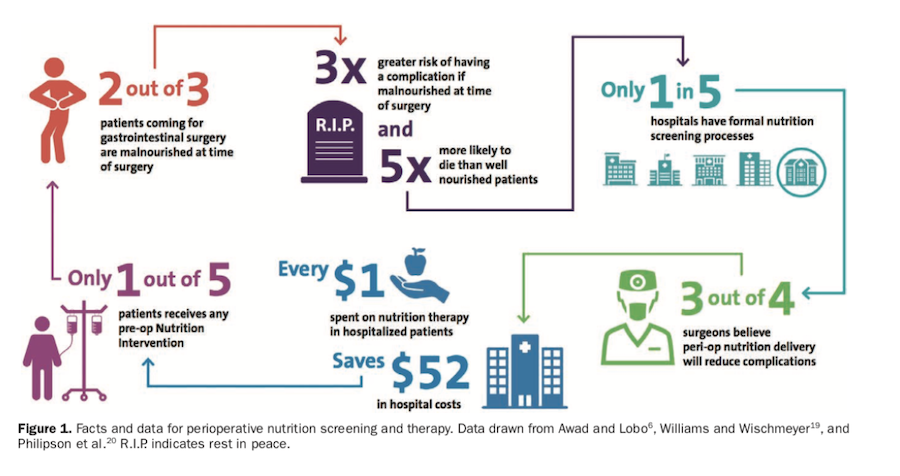
Wow. A big deal to have 20 to 50% of elders at baseline, and then about a third of them become malnourished. So you guys are very busy in the hospital. And how does be malnourished impact outcomes? Why should we be panicked about this? I know we sometimes we think like, oh, they’re really thin or whatever. But now I’m thinking of the patchy score. Being malnourished really increases someone’s acuity, it changes the projection for their outcomes and their level of illness. Why is that?
Megan Dockweiler, MS, RD, CNSC 15:30
Well, malnutrition, like with poor outcomes, but also look at the economic burden. It also it’s an independent indicator of mortality, longer hospital length of stays, higher infection rates, for wound healing, unfavorable outcomes in general, and readmission rates, as well. So it just impacts everything.
Amand Bakko, MS, RD CNSC 15:50
Yeah, the main thing we definitely want to try to prevent, like the wounds, so there definitely increased risk for developing those pressure injuries. And I think the length of stay, it’s one and a half to 1.7 times longer of a malnourished patient versus a regular healthy person.
Kali Dayton 16:07
Well, and how does that impact readmission rates? Yeah, so
Amand Bakko, MS, RD CNSC 16:10
it’s a 60% increased risk and readmission within 15 days.
Kali Dayton 16:14
60% within 50 days, 15 days? Yes, yeah, that is so significant. And I think that plays into this whole picture of being deconditioned, malnourished, deconditioned, their poor functional status, they are at such high risk of being readmitted. But malnutrition plays such a huge role in that. That is, that’s mind blowing. What else is the current research showing us?
Amand Bakko, MS, RD CNSC 16:44
With malnutrition, so basically, disease related malnutrition cost in the United States, anywhere from 147 to 157 billion per year in medical costs. So it’s definitely a financial burden along with the readmission rates, and then just the financial burden of those pressure injuries that develop from being malnourished.
Megan Dockweiler, MS, RD, CNSC 17:05
Yeah. And a study done by Dr. Wishmeyer also said that, like malnourished, malnourished patients added like about $10,000 more to hospital costs to stay two times higher discharge rate to the long term care facility or rehab 1.4 1.4 higher need for home health care, under nourished patients are also more two times more likely to develop pressure ulcers, and the is 3.8 times more likely to impact readmission rates.
Kali Dayton 17:35
So much of this podcast has been focused on discharge disposition, how do we get patients home? I mean, it’s in the title, right? Walking, walking home from the ICU. So we’re trying to avoid Eltech admissions readmission rates. But how did I make it till episode like 90, before we actually talked about really dived into nutrition, we talked about nutrition in the context of preventing muscular atrophy, but also trying to correct even baseline mount nutrition. So what can be done? What do you guys do? And how do we improve upon our response to malnutrition in the hospital?
Amand Bakko, MS, RD CNSC 18:12
Yeah, again, I think it’s just early enteral nutrition. From an ICU standpoint, we if a patient is malnourished, we want them to be initiated as soon as possible on you know, if it’s enteral, the ideal is five days, but that’s five to seven days, that’s more on the general for so when it’s in the ICU, it’s basically as soon as possible, you kind of brought up the you know, being on high flow, that’s something that’s a huge issue, especially obviously, with COVID.
Our BiPAP patients are high flow patients, they’re going to five to seven days without, you know, getting good nutrition, because, you know, technically based on aspirin guidelines, you should be feeding those patients parentally. Whereas some doctors are more hesitant towards that, obviously, fluid status, it’s not recommended to try to quickly feed somebody when taking off the BiPAP Mac mask quickly just because of risk risk of aspiration. So sometimes if those patients can’t get off the BiPAP, they will go five days, you know, getting less than 50% of their needs.
Megan Dockweiler, MS, RD, CNSC 19:13
And to add to that with the BiPAP and TPN. And everything. They think that infection rates is a high thing that is 2030 years old. It’s been disproven multiple times infection rate is not yes, in the old times. It’s with hyperglycemia, which with bundled care of nursing, things like that sterilized care, but now if you have appropriate care and you control things you can it’s not the TPN that’s causing the infections. When we talk about the ICU, we also have to take in consideration again, intubation.
Are they on pressors are they on propofol things that add non calorie nutrition like the purple fall like IV fluids? We have to look at all of that if they’re on pressors how many pressors what’s the dosage rate? Are they trending up trending? down, what’s their lactate? What is their lab status, what is which things all that takes, we take that into consideration. And we want to at least get trickle feeds in there to maintain gut integrity and and reduce oxidative stress and just help with the immunity. So all of that is just we all we just consider that
Kali Dayton 20:24
I didn’t consider that…. and I’m not sure that the whole team considers that. We try to bring the whole team to get that going, right, it takes intensivist to understand, hey, this patient probably needs TPN sooner or later, that respect your your expertise in this and understand the big picture. So what are some of the barriers that you see that your colleagues or yourself have been battling with in the ICU community, in starting enteral nutrition, ASAP on these patients.
Megan Dockweiler, MS, RD, CNSC 20:54
Enteral nutrition is a lot easier to start just because they place like they intubate the patient, and then they’ll place like a tube, it’s when they get excavated is also very hard, because they’ll take the tube out, which we want to keep that in. But parenteral nutrition, again, it’s fluid status, it’s the infection rate thing. And they are concerned whether the five days to seven days is the Aspen guidelines, the new Aspen see Critical Care Medicine guidelines for COVID, on the BiPAP HiFlo, that came out when COVID hit.
And that was when you can start it earlier, especially in the patients that are malnourished. So we normally do two feeds, except that they don’t tolerate the two beads is that the two feeders at the medications is it they have to get a K up is the replacement? Correct. They have to get the imaging, they have to see if they have any other signs of intolerance, like nausea, vomiting, abdominal distension, things like that have to be taken into consideration.
Amand Bakko, MS, RD CNSC 21:57
And I think those struggle is once they’re activated, or if they’re just our patients in the ICU that, you know, they’re not intubated, but they’re just not eating. I think a lot of nurses doctors is just like, we don’t want to place a tube and the patient that’s completely alert and fine. They’re just not eating because they’re sick is fine. But in the ICU, we really got to push for it.
And you know, if the patient is agreeable, then there’s no reason why we shouldn’t place it now if they’re totally against if they’re like, you know, the young patient that doesn’t want that that’s one thing, but we don’t really know sometimes how, how often that question is being asked, you know, if you’re eating nothing on your tray for multiple days, where they offer the to feed, you know, just to make sure or you know, where we consulted, so we can go talk to the patient and kind of, you know, let them know you’re at increased risk for XY and Z are you open to a tube feed, so it’s more so the patients once they’re excavated or thrown modified textured diets, like pureed pudding thick diet, a patient really isn’t going to get much nutrition on that. So can we keep the you know, Angie, and once we excavate them and see how they do with eating.
Megan Dockweiler, MS, RD, CNSC 23:04
And a study shows that even seven days post excavation, adequacy of protein and energy intake was poor, the intake never exceeded like 37 to 55% Of the estimated requirements. So we really push for, to feed and to die together to help meet their needs.
Kali Dayton 23:25
Right? And that’s post extubation. So at that point, they’ve already lost so much muscle. How can you rehabilitate if you’re having 30s to 50s percent of nutrition? That that is a huge barrier to actually rehabilitating and going home. I think the ICU we think two feet there for people that can’t swallow they have severe dysphasia. But you make a great point. That’s not the only indicator for two feeds. But I think culturally we think, okay, they have a tray in front of them speak to clear them to swallow.
They don’t want to eat it’s fine, whatever. And we’re not looking at what’s their caloric intake. I was amazed at here, how many COVID Patients are hypermetabolic? How common is that? You know, we just don’t understand the importance of meeting their metabolic needs, even when they can swallow what what a dietitians wish that the ICU community knew or would actually implement in their culture and practices.
Amand Bakko, MS, RD CNSC 24:28
I think first and foremost, just the importance of nutrition. You know, we base our documentation off of what the nurses document and a lot of times the nurses don’t document how much the patient is eating. And we know they’re busy and you know, nurses have a lot on their plate. But if that’s not something that they’re thinking about, like oh, I should document how much this patient is eating. They’re not going to think about how do I get this patient to eat more. So that’s just something that is why we’re at rounds. You know, at rounds, we’re always like How’s the patient eating what percentage They have a supplement, are they drinking it? So that’s definitely an issue.
Kali Dayton 25:05
And IT teams have a culture where dieticians can’t interject themselves and aren’t involved in rounds. And nutrition isn’t being tracked, how much are these patients suffering because of it. And again, also much comes down to culture. I mean, we have these great disciplines about this expertise, all this research coming out. But if we can’t apply it, it’s all for nothing. Right? So what are some of the barriers you find patients come in that are malnourished? And then you get excited, and you’re able to start giving them nutrition? What happens then? And how does that impact critical illness?
Amand Bakko, MS, RD CNSC 25:39
I would think barriers would just be placing that too, if it’s needed, you know, maybe not, like I said, we come from an ICU where we basically see our ICU patients within 24 to 48 hours. But I know in the past at my previous hospital, like we would be going on day five to six, where, you know, we didn’t sometimes always go to rounds everyday for whatever reason. And we would come across these patients, or they get transferred from another floor where they have the poor appetite.
They’ve been here for a week. Now they’re in the ICU. And sometimes I feel like the nurses are not thinking like, oh, they just got in the ICU, but they’ve already been here for seven days. So we need, we can’t wait another four to five days to think of what is our intervention going to be like if this patient needs to to feed they needed to feed. And also,
Megan Dockweiler, MS, RD, CNSC 26:27
if you go that long, we also are at risk of refeeding syndrome, which is high, it caused a couple of intubations within my patients couple of times. It’s a complication, including like severe electrolyte abnormalities that can cause like heart failure and respiratory failure and even death. So most of the time, you hear us asking, Can we check a fast? Can we get some time in how the other because the lights are normally we’ll all we look at and phosphorus phosphorus is the highest one, that’s the most important indicator. So that is also a significant complication if they are prolonged without any nutrition.
Kali Dayton 27:05
And then equally, it’s life threatening.
Amand Bakko, MS, RD CNSC 27:07
Yeah, yeah. And I think we have issues too, of course, with our surgery patients, those people that come in with bowel obstructions that they think they’re just going to resolve. And we’re now on day six, and they’re still NPO. And now they’re going for surgery, you know, they just went those six days in house with you know, clear liquids, and they probably weren’t eating well, like a week before coming in.
And so now they’re going into surgery, then they’re going to have their post op phase where we’re not going to feed them right away. So those are the patients that we really want to try to get the TPN started parenteral nutrition, something because they’re going into surgery, malnourished, and that’s a huge issue.
Megan Dockweiler, MS, RD, CNSC 27:44
And then as also like where the D5s at 100 start and then that’s a lot of carbohydrate dextrose at once, and then you’re getting so many calories that they will go into refeeding. So that’s why we kind of started earlier started sooner, so that we can avoid that complication, and then provide the amino acids again to protein to help at least preserve lean body mass sets there, because protein provision is the is the most important and it’s more important than just even trying to meet their calories.
Kali Dayton 28:11
Yeah, how do you stay calm when you get consultations when it’s that late? Right. And when you know you, you’re so well informed of the big picture and the reality of what’s going on because I again, it comes from kind of the nursing side, nutrition wasn’t a huge part of my education, not necessarily a huge part of our focus yet. And I think sometimes we think if patients are obese or have a higher BMI that we’ve got days to spare, we think about losing some extra weight won’t be a big deal. So why is it a big deal? What’s the first to go and why is this important in obese patients?
Amand Bakko, MS, RD CNSC 28:44
It is very important. Yes, this is
Kali Dayton 28:48
you guys are shattering.
Megan Dockweiler, MS, RD, CNSC 28:51
Record. First off, they took they can coexist. Malnutrition and obesity can coexist they, they mainly have more fat stores. So without inadequate nutrition patients lose their muscle first, like the weight this weight loss is detrimental. And they also metabolize lean body mass at higher rates. So they obviously lose lean body mass increased amount.
Kali Dayton 29:17
So I’m thinking of some of our, like 400 500 pound patients, right? In my mind, those are the most important to be mobilizing early for even just for the sake of the staff. Because if they become that we can get conditioned. It’s a huge hazard for everyone. And I’m not sure how we expect them to survive if they lose that muscle. So how lethal is it to assume that they can go days without eating or being fed? And then like you’re saying the first thing to go, is there lean muscle?
Well, we need that muscle on those big bodies, to be able to have them off the ventilator and to move on their own and not to be a hazard to our team as we’re trying to push on them or turn them off. Remove them after they’ve been deconditioned. So, like so many things on this podcast, that is goes onto the list of complete opposite, you have just debunked a huge myth within the medical community. So our perspective on obesity needs to change.
Amand Bakko, MS, RD CNSC 30:19
Yeah, and with malnutrition and the patient who’s obese, like Megan said, they can’t coexist, because remember, when we identify malnutrition, it has, it’s based on weight loss. Obviously, those people who come in with a 400 500 pounds, they can have weight loss, we don’t know anything about them by looking at them.
So it’s weight loss, you know, if they’ve been eating poor, so that’s what we’re going to look at. And physical signs of muscle wasting, and they have such high protein needs to maintain that body mass. So if they’re on, you know, if they’re not intubated, we have, you know, certain supplements, high protein supplements that we give them, just because we need they’ll never get the protein that they need from the hospital tray. That’s, you know, the tiny hospital tray with like, half a portion of meat.
Kali Dayton 31:03
No, I, yeah, it’s not adequate at all, especially when we’re talking again, about these COVID patients, even just the respiratory rate is so high, that hypermetabolic just because the inflammatory process, we fail to take that into account when we’re just looking at a patient that we assume has had nutrition or has been eating throughout their lives. How does like, why is protein so important? And how does that impact even just, again, the respiratory drive respiratory function, when we’re talking about liberating patients from the ventilator? Why would protein and nutrition be so important in that discussion?
Amand Bakko, MS, RD CNSC 31:40
Yeah, I mean, it definitely just involves our muscles. So just having the muscles to breathe and losing the muscles to swallow. So if they’re getting off ventilator, if they’re going to have dysphasia, they can lose that muscle, you know, if if they have dysphasia, it could be because they lost that muscle and their vocal cords. So they’re trying to, you know, eat and having issues with dysphasia. So that’s a huge thing, a huge thing with the muscles with breathing, and oh, my didn’t have some good stats in here about protein.
Megan Dockweiler, MS, RD, CNSC 32:11
Yeah, patients who received adequate protein are more likely to be weaned from the ventilator and had an over lower ICU and overall hospital mortality and greater 60 days survival than those who did not.
Amand Bakko, MS, RD CNSC 32:23
And we, you know, when we’re estimating the needs for the ICU, they baseline have higher protein needs, because they’re in the ICU, they’re in a critical illness phase. So already, they have higher needs. And then we the protein needs differ based on BMI and their weight. So someone who has a little bit higher BMI will have a little bit higher protein needs.
And then we put into account everything if they have wounds, if they’re septic, that all increases the protein needs. So we’re changing protein needs. We have you know, for our intubated patients, we have our protein modules modular so we’re using those a lot with those patients.
Kali Dayton 33:01
Wow, I’m so glad you guys are there. Because it is such a niche. It’s you’re so specialized in this and I’m thinking about the awakened walk in ICU, their pressure ulcer rate is like less than 1%. A lot of patients are able to eat sometimes the very next day after we can intubated for weeks. Sometimes it takes a few days, sometimes it takes longer, but on average, they’re eating and swallowing, they’re walking out the doors.
But when they discharged from the hospital, I thought a lot about that was from early mobility, which clearly clearly it is, but dieticians are also very involved there. They are very prompt and aggressive about nutrition. And I did not appreciate the role that that played in those kinds of outcomes that they’ve had. Well, how else are outcomes impacted?
Amand Bakko, MS, RD CNSC 33:50
I think just muscle wise, I’m getting the protein in we have our patients that have tricks and pegs. So getting that nutrition in once they have the PEG tube and that really helps them recover
Megan Dockweiler, MS, RD, CNSC 34:04
Over feeding and under feeding we have to be aware of just because it can prolong time on the ventilator with the co2 production when we’re over feeding them that will prolong it. But because we are also hypercaloric Lee feeding them. So based on that they will inherently lose some weight.
Because what that’s why protein provision is the most important to reserve that lean body mass preserve that lean body mass. But once they’re off event, once we’re going between leading trials and or and or they get a trade and can go on high flow or root trip to room air, then we ramp those speeds back up and to meet their actual needs. But that’s why protein going back to what we discussed already is the most important and independent of caloric intake because we automatically always hypercaloric We feed our intubated patients
Kali Dayton 34:56
Interesting…. and I’m thinking to how much of that The tracheostomy rates that we’re seeing right now it’s COVID patients could also be prevented with nutrition if these patients spend, however long days, weeks on high flow or BiPAP, and then are not getting the nutrition they need. They’re not getting mobilized, how much does that lead into them being intubated.
And then finally they get intubated. And then finally they start getting fed because they’re intubated. And at that point, the diet and then they’re not moved to the canal, the sedation, diaphragm has had so many assaults to it. But if we really nourished the diaphragm, how much more successfully, could they be extubated and they could swallow and they wouldn’t need peg tubes, they wouldn’t need the tricks and they’d be able to just move on with life.
Amand Bakko, MS, RD CNSC 35:45
Yeah, and I think one of the issues I don’t know if I reset this, but is these COVID patients that come in, they’re usually already in a malnourished state poor intake, they’re usually losing weight. Some of these COVID patients we seen their diagnosis was like three weeks ago. So we’re talking three weeks of having that poor appetite, the taste changes that go along with it by once they are intubated, if they, you know, get intubated, and we can start to feeds.
You know, again, nothing against nurses. But sometimes the feeds get paused or they get turned off for if they’re going for procedure. If they’re NPO. For some reason, then, yeah, for pruning, like pruning is a huge thing where we have to change the rates, and they usually are not getting their full calorie needs when they’re pruning because when they are prone, it’s what we do at our facilities at triple rate. And then we ramp them up to a higher rate once they’re supine, but they’re only supine for four hours. So it’s not that much nutrition.
But there’s a lot of things that can interrupt the feeds, Meghan was talking earlier about presser so if they’re on multiple pressors, it increases the risk of gut ischemia. So we’re not feeding when someone is on high dose pressors, three pressors. And that can go on for a couple of days. So sometimes we initiate parenteral nutrition if it’s appropriate, but sometimes it’s just a waiting game of when they can get off of them.
Megan Dockweiler, MS, RD, CNSC 37:05
And a couple episodes back, you’re talking about how like they were using propofol but like that one facility or your facility? Does I IV ws with propofol, which I was like that would be so much better if why are we feeding the entire body mass, you know, especially for those patients who are have a higher BMI, we don’t need to feed them. And then because certain protocols that like 100, that’ll meet 100% of their calorie needs and 0% of their protein needs.
And then we have increased risks of like higher triglycerides, like things like like liver injury. And that’s what we have to take in consideration to but we can’t overfeed because that means time on event, things like that. So it’s a balancing act. And it’s trying to can we lower the profile a little bit like we get it, we’re not the doctors or nurses, the ones that are touching the patients, the ones that are in care directly with them. But we try our hardest to push you in a direction where we can at least meet their needs adequately, and prevent what we know we can prevent.
Kali Dayton 38:10
And I wish I understood these things before I remember as a nurse, the dietician asked me in rounds where the feeds pause, how long were they pause for? And I was like, I don’t know, we walked in, we went to see T and then I can’t keep her I don’t know how long. But why are you asking me I go into when I could, you know, just it was just another thing to keep track of it was just but now I see why that is your business. That was extremely important.
Megan Dockweiler, MS, RD, CNSC 38:37
There’s a lot of protocols that are out there. There’s like volume based to feed. So it takes it’s a nursing driven protocol, mainly because the nurse has to say you’re off feeds for two hours or you’re super pro or you’re down for a test. How many hours have you not fit that patient and then you kind of have to do a little bit of calculation to put say they were at 50 miles an hour, then for the rest of the day, it’d be 80 ML is an hour to ramp up to the calorie needs they need for that day.
So there are protocols out there that help with that. We’re trying to implement certain we’ve got the early enteral nutrition protocol and a little bit here, but we’re working towards maybe volume based. So there are things that dieticians are looking at that can help. It’s just the process
Amand Bakko, MS, RD CNSC 39:21
is a multidisciplinary approach. So
Kali Dayton 39:23
no, absolutely, yeah. That’s nice that you come from a team that already has that process ingrained in your culture. And that’s what allows you to move forward and allows you to call in an eight F bundle meeting. And to get things going I just keep thinking how can we implement the ABCDEF Bundle. How can we have these outcomes if we don’t bring dieticians to the table?
You should be best friends with the nurses and the physical therapists and you’re the ones that are going to facilitate all of those goals that they’re working towards. You know, physical therapists are fixated on the muscles and the physical function. Wouldn’t be nice or neat if they could ask Hey, has this patient had a dietitian consultation, and help facilitate that process as well be thinking about it as well. Everyone should have a right to not intrude on each other’s disciplines, but understand what each other does, and know how to best utilize each other. And I think you have every right to be pulling together that that meeting for the ABCDEF bundle and be calling that everyone together to do that.
And I’m so glad that your team is excited to do that. I hope to be able to support you guys. However, I can keep us posted on your successes and your updates and your process. I know it’s a crazy time. But I appreciate that you’re doing that even during this crazy time, because this is when it’s especially Central. What last thoughts would you share with IC community? What What’s your last invitation to us?
Amand Bakko, MS, RD CNSC 40:50
Well, one thing that you kind of said is our whole huge thing is consult a dietitian. If you see a patient like well, that patients really small they look tiny consults with dietician, they probably have some weight loss. I mean, we see patients for so many reasons, CHF, diabetes CKD. And most of those patients have those things going on when they come into the hospital. So honestly, we could probably see every patient, every patient probably needs our help.
So consult us know that we’re the experts with nutrition support. So you know, I don’t know if sometimes doctors or nurses are not afraid but hesitant to do TPN or enteral nutrition because it’s more work but they don’t have to do anything, just put the consults in the dietician will do everything will manage everything. So that’s huge. And then our last final note is that albumin is not an indicator of malnutrition. Every dietitian I’m sure will be happy to hear that but you know, amount of albumin is not an indicator, we get counselors all the time, it’s based on weight loss, and you know, PO intake for malnutrition. An
Megan Dockweiler, MS, RD, CNSC 41:55
and our last thing also is that everybody is human at the end of the day, and they should be treated as such, doesn’t matter their size, BMI, anything, even in the ICU when they’re critically ill, but regular floor patients, weight loss should never be a goal and the hospital and just
Amand Bakko, MS, RD CNSC 42:15
A dietitian should not be consulted for it. We’re here to help our help our patients get nourished for, you know, to help their disease state, we want to make sure they’re getting enough nutrition, we never want to take away nutrition. So we do get weight loss consults, so not appropriate in the acute setting.
Kali Dayton 42:32
Oh, such good points. And you tie perfectly into the whole theme of humanizing the ICU, that you are there to make sure that they stay functional human and survive. And it can’t and won’t happen the way it needs to happen without your involvement as dieticians. Thank you so much. I’m so excited for future collaboration. And if it’s okay, though, to put your contact information if people want to reach out with questions, I think you’re just powerful resources. Thanks for all you’re doing and keep up the awesome work.
Megan Dockweiler, MS, RD, CNSC 43:04
Thank you! We’re excited.
Transcribed by https://otter.ai
SUBSCRIBE TO THE PODCAST



