SUBSCRIBE TO THE PODCAST
We say we respect patient autonomy. We provide patients or families informed consent prior to intubation. Should patients and families be warned of the risks and repercussions of sedation and immobility? When sedation is nonessential, should patients be given the choice to be comatose or awake and moving?
Episode Transcription
Kali Dayton 0:19
If you haven’t listened to the podcast from the beginning, I strongly encourage you to do so before proceeding with this episode. Without context, this episode may be very upsetting. Even if you’re current on the episodes, this may ruffle some feathers.
Today I want to talk about patient autonomy. It is so sacred. One of my favorite perks of having patients awake on the ventilator is that we nor the family have to guess and wonder what they want. They get to call the shots. Many of our own ICU community say cool if it was me, I would want to be sedated. Totally fine, if they are informed of the risks and the options, and then given a choice.
Again, there are situations in which sedation is actually essential. intracranial hypertension, seizures, open abdomen some drug toxicities are the most severe alcohol withdrawal, etc. Even when there is not an option to keep a patient awake and moving, do we warn the patients and families of the repercussions they may suffer?
When a patient discharges with residual kidney injury or changes to medications. We have them follow up with outpatient providers. Yet do we tell our patients you had ICU delirium and may suffer symptoms of PTSD or have cognitive deficits?
Do we provide psychological and cognitive therapies to follow up with after discharge?
And all the other occasions in which the patient has been administered automatically after every intubation just out of cultural habit?
Are we being straight with patients and families? What if we told them the truth about sedation and immobility and provided the option before intubation? What if it was part of the waiver?
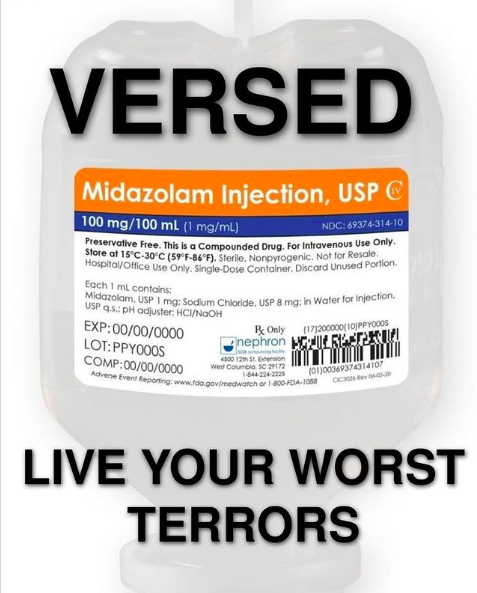
What if we told our COVID patients, “Hey, your lungs are getting worse to the point of needing a ventilator. So we’re going to damage your brain and muscles to this will probably contribute to other organ failures and your eventual death. I can tell you hate the ICU. So we’re going to psychologically send you back to the worst moments of your time in Iraq.”
Listen, there are always risks and side effects of treatments. We do informed consents all the time. This provides autonomy for the patient and protection for providers. As a legal consultant, I have frequently told clients, ‘I am so sorry you suffered this complication. But, you know, infection was a risk listed on the consent you signed prior to your ERCP.”- And that was for an essentially, intervention. sedation is rarely essential and comes with life altering risks, and yet we automatically give it without informing patients and families.
We are not allowing them to have options and make informed decisions. I would suggest that our consent forms prior to intubation are not adequate or fully transparent. If we truly respected patient autonomy, we would be honest and clear with him prior to intubation. Our informed consent would include the option for or against an essential sedation.
It would say something like, “Sedation is an optional addition to mechanical ventilation. It comes with the risks of dying in the ICU or after the ICU, infection, pressure sores, blood clots, delirium, ICU acquired weakness, more time on the ventilator more time in the hospital, tracheostomy, discharged from hospital to rehabilitation center or nursing home ICU PTSD, Post ICU, dementia, or cognitive dysfunction, depression, being readmitted to the hospital and ICU, post intensive care syndrome, losing the ability to walk or breathe independently, and decreases your chances of discharging home from the hospital being able to walk upon transfer in the ICU, returning to work, or resuming your baseline quality of life.”
Just like with any procedure that has special risk factors specific to a patient, we would also specify with patients that have psychiatric histories and baseline PTSD, that they may be at more risk of reliving their worst traumas.
Studies for all of these statements are on the blog. If you’re feeling defensive, or hating this concept, please pause and do some introspection. Why would this kind of transparency, be bothersome or uncomfortable to us?
When we tell families that we are doing everything we can to help patients survive, yet we are deeply sedating everyone, even with the evidence that that increases mortality. Are we telling them the truth?
What if the public knew how different their outcomes could be depending on the hospital, in the same city or even the unit within the same hospital, simply because of their sedation and mobility cultures. I worked in the city where in one unit 98% of survivors discharged home and that was compared to a neighboring hospital with patients of the same Apache score, and only 46% of those survivors discharged home. So from the “Awake and Walking ICU”, a few blocks down the road, there’s no way you would open your eyes on a ventilator.
A few miles south, you’d get sedation vacations, but not would not likely stand up or walk. A few miles to the east or the west, you get to walk on ECMO in one unit, but hardly sedation vacation on the ventilator in another unit within the same hospital.
Emergency Services transport patients to specific facilities. For certain cases- suspected MI go to where there is a cath lab. Traumas go to trauma centers. What if respiratory failures suspected of needing prolonged time on a ventilator had the choice of going to facilities that had the best management of patients on ventilators?
Knowing what you know now about how different outcomes are depending on sedation practices. Wouldn’t you want the choice? What if insurances held us liable for ICU acquired weakness when we inappropriately sedate and immobilize just as I do with infections and pressure injuries?
Medicare doesn’t cover expensive repercussions of poor care, such as hospital acquired infections. So what if hospitals were not reimbursed for preventable tricky ostomies prolonged stays or penalized for ICU acquired weaknesses or discharges to LTACHs. I have been a consultant on cases with survivors trying to sue for far less injuries than what we cause with sedation and immobility.
Again, none of this is to demonize anyone. Yet I cannot fulfill my objective of the podcast and advocate for patients if I don’t address their right to be informed and be active participants in choosing their treatment and outcomes. We should not be withholding this information for from them. Not only are we failing to warn and support them in recovering from the damage we have caught, we are failing to give them the opportunity to avoid it.
I know it is a minority of the ICU community that is even aware of this research and the reality of our practices. Get as one of the few that know what is going on. I am tired of this being our dirty little secret. We need to be involving our patients and their families, and the evolution of critical care medicine. We need to honor the right to know before we proceed with automatic deep sedation and immobility. Someone recently said to me that they are tired of traching and pegging all their COVID patients and seeing their mortality rates in the 90’s.
We should be sick of it. We know how to improve mortality rates. We know how to improve outcomes and prevent suffering. families and patients have the right to know as well. If we cannot provide that kind of care, then we should be transparent. We would expect that at any surgeon doing surgeries on us or our loved ones. So I know that was a lot and thank you for listening to such a rogue ramble
Transcribed by https://otter.ai
References:
- Shehabi, Y., Bellomo, R., Reade, M. C., Bailey, M., Bass, F., Howe, B., McArthur, C., Seppelt, I. M., Webb, S., Weisbrodt, L., Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators, & ANZICS Clinical Trials Group (2012). Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. American journal of respiratory and critical care medicine, 186(8), 724–731. https://doi.org/10.1164/rccm.201203-0522OC
- Tanaka, L. M., Azevedo, L. C., Park, M., Schettino, G., Nassar, A. P., Réa-Neto, A., Tannous, L., de Souza-Dantas, V. C., Torelly, A., Lisboa, T., Piras, C., Carvalho, F. B., Maia, M., Giannini, F. P., Machado, F. R., Dal-Pizzol, F., de Carvalho, A. G., dos Santos, R. B., Tierno, P. F., Soares, M., … ERICC study investigators (2014). Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Critical care (London, England), 18(4), R156. https://doi.org/10.1186/cc13995
- Lin, S. M., Huang, C. D., Liu, C. Y., Lin, H. C., Wang, C. H., Huang, P. Y., Fang, Y. F., Shieh, M. H., & Kuo, H. P. (2008). Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. Journal of critical care, 23(3), 372–379. https://doi.org/10.1016/j.jcrc.2006.09.001
- Rello, J., Diaz, E., Roque, M., & Vallés, J. (1999). Risk factors for developing pneumonia within 48 hours of intubation. American journal of respiratory and critical care medicine, 159(6), 1742–1746. https://doi.org/10.1164/ajrccm.159.6.9808030
- Cox, J., Roche, S., & Murphy, V. (2018). Pressure Injury Risk Factors in Critical Care Patients: A Descriptive Analysis. Advances in skin & wound care, 31(7), 328–334. https://doi.org/10.1097/01.ASW.0000534699.50162.4e
- Minet, C., Potton, L., Bonadona, A., Hamidfar-Roy, R., Somohano, C. A., Lugosi, M., Cartier, J. C., Ferretti, G., Schwebel, C., & Timsit, J. F. (2015). Venous thromboembolism in the ICU: main characteristics, diagnosis and thromboprophylaxis. Critical care (London, England), 19(1), 287. https://doi.org/10.1186/s13054-015-1003-9
- Pandharipandh, P., Shintani, A., Peterson, J., Truman, B., Wilkinson, G., Dittus, R., Bernard, G., Ely, W.(2006). Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients, Anesthesiology, 104. Retrieved from https://pubs.asahq.org/anesthesiology/article/104/1/21/7483/Lorazepam-Is-an-Independent-Risk-Factor-for
- Yang, J., Zhou, Y., Kang, Y., Xu, B., Wang, P., Lv, Y., & Wang, Z. (2017). Risk Factors of Delirium in Sequential Sedation Patients in Intensive Care Units. BioMed research international, 2017, 3539872. https://doi.org/10.1155/2017/3539872
- Pereira, J. V., Sanjanwala, R. M., Mohammed, M. K., Le, M. L., & Arora, R. C. (2020). Dexmedetomidine versus propofol sedation in reducing delirium among older adults in the ICU: A systematic review and meta-analysis. European journal of anaesthesiology, 37(2), 121–131. https://doi.org/10.1097/EJA.0000000000001131
- Vanhorebeek, I., Latronico, N., & Van den Berghe, G. (2020). ICU-acquired weakness. Intensive care medicine, 46(4), 637–653. https://doi.org/10.1007/s00134-020-05944-4
- Strøm, T., Martinussen, T., & Toft, P. (2010). A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet (London, England), 375(9713), 475–480. https://doi.org/10.1016/S0140-6736(09)62072-9
- Brook, A. D., Ahrens, T. S., Schaiff, R., Prentice, D., Sherman, G., Shannon, W., & Kollef, M. H. (1999). Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Critical care medicine, 27(12), 2609–2615. https://doi.org/10.1097/00003246-199912000-00001
- Pun, B. T., Balas, M. C., Barnes-Daly, M. A., Thompson, J. L., Aldrich, J. M., Barr, J., Byrum, D., Carson, S. S., Devlin, J. W., Engel, H. J., Esbrook, C. L., Hargett, K. D., Harmon, L., Hielsberg, C., Jackson, J. C., Kelly, T. L., Kumar, V., Millner, L., Morse, A., Perme, C. S., … Ely, E. W. (2019). Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Critical care medicine, 47(1), 3–14. https://doi.org/10.1097/CCM.0000000000003482
- Davydow, D. S., Gifford, J. M., Desai, S. V., Needham, D. M., & Bienvenu, O. J. (2008). Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. General hospital psychiatry, 30(5), 421–434. https://doi.org/10.1016/j.genhosppsych.2008.05.006
- Nelson, B. J., Weinert, C. R., Bury, C. L., Marinelli, W. A., & Gross, C. R. (2000). Intensive care unit drug use and subsequent quality of life in acute lung injury patients. Critical care medicine, 28(11), 3626–3630. https://doi.org/10.1097/00003246-200011000-00013
- Wilcox, M. E., Brummel, N. E., Archer, K., Ely, E. W., Jackson, J. C., & Hopkins, R. O. (2013). Cognitive dysfunction in ICU patients: risk factors, predictors, and rehabilitation interventions. Critical care medicine, 41(9 Suppl 1), S81–S98. https://doi.org/10.1097/CCM.0b013e3182a16946
- Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011 Feb;39(2):371–9. doi: 10.1097/CCM.0b013e3181fd66e5. PMID: 20959786.
- Hopkins, R. O., Mitchell, L., Thomsen, G. E., Schafer, M., Link, M., & Brown, S. M. (2016). Implementing a Mobility Program to Minimize Post-Intensive Care Syndrome. AACN advanced critical care, 27(2), 187–203. https://doi.org/10.4037/aacnacc2016244
- Rawal, G., Yadav, S., & Kumar, R. (2017). Post-intensive Care Syndrome: an Overview. Journal of translational internal medicine, 5(2), 90–92. https://doi.org/10.1515/jtim-2016-0016
- Kamdar BB, Suri R, Suchyta MR, Digrande KF, Sherwood KD, Colantuoni E, Dinglas VD, Needham DM, Hopkins RO. Return to work after critical illness: a systematic review and meta-analysis. Thorax. 2020 Jan;75(1):17–27. doi: 10.1136/thoraxjnl-2019–213803. Epub 2019 Nov 8. PMID: 31704795; PMCID: PMC7418481.
- Nelson, B. J., Weinert, C. R., Bury, C. L., Marinelli, W. A., & Gross, C. R. (2000). Intensive care unit drug use and subsequent quality of life in acute lung injury patients. Critical care medicine, 28(11), 3626–3630. https://doi.org/10.1097/00003246-200011000-00013
SUBSCRIBE TO THE PODCAST



 When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team.
When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team.
