SUBSCRIBE TO THE PODCAST
Kali talks to Susan East, three-time “ARDS” or “ARDS” survivor, about acute respiratory distress syndrome – the most severe forms of lung failure.
Episode Transcription
Kali Dayton
Hello, and welcome back. Today we’re going to talk to Susan East who is a three time “ARDS” or “ARDS” survivor, which represents acute respiratory distress syndrome, which is one of the most severe forms of lung failure that occurs from the lungs filled with fluid in response to conditions such as pneumonia and sepsis.
These patients require prolonged time the ventilator, and sometimes have to be paralyzed and lay face down for days. These are the patients that receive the most days on the ventilator the most sedation become the most delirious and the most immobile, they therefore, can have the poorest long term outcomes. So we’re fortunate to have Susan with us today to give us a real insight into survivorship of art. Susan, thanks so much for joining us today.
Susan East
Well, thank you for having me.
Kali Dayton
Tell us about your experience with ARDS.
Susan East
Well, I’ve had our three times. I’ve had it in 2008 2014, and then in 2017. So that’s probably not the norm for most people. That that’s been my experience with ARDS.
Kali Dayton
Wow. Wow.
Susan East
Yeah. So the first I thought it was back in 2018 and a and I had no clue what ARDS was. I had a sinus infection, or like I thought was a sinus infection on Monday, June 30. And my husband went with me to the doctor, just I can always go through with it. And they diagnosed me the sinus infection gave me a cortisone shot sent me home with a, like a steroid pack. And, you know, he said, I’d be better in a couple of days. And I never wanted to be sick. So I didn’t think anything of it. And my daughter lived down the street from me. And she was in nurse anethestist school at that time, she was she was working as a ICU nurse.
And so she had stopped by my home Wednesday evening for something and she noticed that I was very irritable and get out of sorts. And she told my husband something wasn’t right. And so she just thought that I didn’t look right in her. And I thought I was just real tired. So the next day, she came by to check on me. And when she came by, I was blue. Blue. I was sitting up. And what’s really odd is, I wouldn’t let her call 911. I was awake enough to talk to her. And so I told her, “No, you’re not calling 911.” I said, “If I let you run me up to my doctor, he will give them exam and do a chest X ray, will you please bring me home and leave me alone?” Like kind of relationship.
And so she agreed. And because she knew that’s all she needed was just to get my foot in that door. And so when I got there, when I walked in the doctor’s office, that that exhausted me and I collapsed, and they started taking off Palafox with every thing they had in there, and they were all reading like 4243 rows, like, Oh, these things are bright there. So they called my mom line even though the hospital was right next door. And they did a blood gas in the headaches shown a lot of time I did the blood gases they caught up to maybe 46. But it was right. Oh my gosh, she had reason for concern. And so, you know, I was very, very sick, sick and oxygen deprived. And but nobody knows.
And they just didn’t know what was wrong with me. And rushed me over to the hospital and put me straight in ICU and took me on BiPAP which was a nightmare. I’d rather be on a ventilator any day than BIPAP. They just felt like it was suffocating me. You know, I just didn’t like that feeling. Right. You know, I don’t know, but I just knew, you know, I could tell I was really really sick. But I didn’t know what was wrong. So anyway, that went on for about probably about 13-14 hours with no success.
You know, it’s like, any time you know, my family stay with me around the clock and ICU because anytime if they weren’t somebody wasn’t there keeping me awake? I would doubt no it soon as I does, my SATs dropped really low. So it wasn’t working. And the doctor came in and tell my family there’s so we’re going to have to, you know, put her on a ventilator. And even in my family, even my daughter was in school to be a nurse anesthesist. She was a nurse anethesist and wasn’t real familiar and to her mother, so it’s a whole different situation. Oh, yeah. So they weren’t gonna, you know, medically put me on vent. And my family agreed and signed the paperwork. And so I was in a medically induced coma for probably six days. And while that transpired, you know, the strangest of things happen. That’s when I experienced delusion.
In terrible, terrible during that I will never forget as long as I live. And that’s why I never want to be sedated again, the rest of my life. There’s other reasons too. But that’s, that’s a lot of it. So you weren’t not only pardon me,
Kali Dayton
So you weren’t sleeping under the sedation.
Susan East
I was asleep. But I was. I was awake. It’s really hard for me to explain. I could hear what was going on in the room. I mean, I was sedated that I was having, like my father-in-law was diagnosed with cancer. And my husband and my daughter, were talking about it in front of me because I thought, well, she’s in a, you know, a medically induced coma. She can’t hear or saying, I have every single thing that was sick.
Kali Dayton
Oh, wow.
Susan East
And when they brought me out of it, my daughter was there. My husband wasn’t at that time. And I asked her what kind of cancer just you know, your your grandfather had. And she looked at me like, she’d seen a ghost. And she said, Mom, you are on some strong drugs. He doesn’t have cancer. Well, I knew I knew that was as far as I was going to get with her. So let it go on. My husband got their, you know, I asked him, I said, “Look, I heard y’all talking.” And he told me the truth. And so they were everybody was blown away. And there were other things I heard too. And I could feel my husband and I tell him, I said, You kissed me right here everyday, didn’t you? He said, Yeah. And so you know, and that’s why I tell people now, maybe everybody doesn’t hear, but you don’t know what people are hearing. So please be cautious. Right, what you talked about?
Kali Dayton
And could you understand what was going on? You said you were having delusions and hallucinations?
Susan East
Yes.
Kali Dayton
What was that? Like?
Susan East
They were terrible. That delirium, and I’m not, I’m sure that was from those strong drugs. I was laying there and I couldn’t move, you know. And I felt like I was pinned down. But I could, I knew I was in the hospital bed. And I could see babies floating all around me. And there was a fire around me and I couldn’t help these babies. And it was the most terrifying feeling in the world behind there. There’s a fire. And um, I’m worried about these babies, I can’t get to them. And they’re gonna die. And it was it was horrible.
I mean, it was traumatic. And and my daughter said my blood pressure would go up and down, up and down. And I said I can only imagine because what I was what I was going through. And you know, when I when I nobody, you know, at first, like, nobody would believe me, my daughter did and my family did that nobody else would. And I have it in my chart to never be sedated unless it is absolutely 100% necessary.
Kali Dayton
Wow.
Susan East
No matter what. I am not afraid to be on a ventilator, but do not sedate me. Do not sedate me. The sedation is what I’m afraid of.
Not only that, to me, it’s harder to to get back to where you need to be by not being. I mean, I was in oh eight I was then at a total 28 days. I think it was six days. I was medically induced the rest of the time I was late, and I mean awake to where as soon as I got out of it that my family had me moved to a trauma center and And they, they brought me out to meet me.
They had I was, they put me back in a medically induced coma. And as soon as I got to the Louisiana State University Trauma Center, they brought me right out of it. And I was never put back under again. And I mean, I was awake is awake as I am now. As soon as I got strong enough, I started journaling and writing when I was intubated. While I was intubated, yes.
Kali Dayton
Oh, good. What did that do for you?
Susan East
Mentally, it made me feel like a normal person. It made me cope with, I felt normal. I didn’t feel like somebody who was laying there in a vegetative state, or someone who couldn’t do for herself, that I felt like I can overcome this. This is not a death sentence, this is something that I can get better and I can overcome this, this is not going to overcome me. It gave me more control of it.
Kali Dayton
And you were able and allowed to participate.
Susan East
Yes. And that was so important. Because there came a point in time, probably into my fifth week. You know, good days, bad days, where my doctor came in one day, and she said, We, I need to do a long biopsy, just to see if I can find something. And my husband and my daughter and my son in law, he he was off and working there. And they said “no”.
And I looked at the doctor because I was on a vent. And I said, I pointed to me. And she said, because I didn’t have a tablet. And for me, I just pointed me, she said, “Can you sign”? she said, “absolutely”.
I said, pointing my thumb up. I said, “Okay”, I said and get like, “fine”. She brought me the paperwork. And I sat there and signed it in front of everybody. And they prepped me and took me down.
Ya know. And that was very important to me. I wanted to be in control. Yes, I mentally was fine. And because of that, when they did it, they they found like a sack of fluid when they cut into me. And it released it. And I started getting better immediately. And that, you know, my family. And that’s what I’ve told my family since then, because you have had had it twice since then. You’re not in control of me, unless I can’t be in control of me. I’m in control of me.
Kali Dayton
And they stopped taking away the control. Or they give the control back to you when they allowed you to wake up.
Susan East
Exactly. It’s my Savion
Kali Dayton
I love it. Were you wanting
Susan East
to pay, people have to feel that patients have to feel that in order to feel strong. And to get better.
Kali Dayton
They have to be able to do it for themselves as well. Yes, absolutely. And there’s some dignity that’s preserved in that correct. While you were awake there, were you mobile were you walking?
Susan East
No, I, I literally had a tube and every opening in my body, except my ears. That came and tried to get me up a couple of times. But I had been flat on my back for so long, I couldn’t stand up, I just crumble. And that was the unfortunate thing in oh eight that they didn’t work on mobility as much. So when I was discharged, I was discharged to a rehab facility via ambulance, because I couldn’t stand up. And so when I was sent to this place, I mean, at that point in time, I could get up on a walker and go to the bathroom, but they wouldn’t let me. So I was in this facility. And only two times a day for maybe 20 minutes, 30 minutes, they would take us down this room and exercise like eight of us at a time, and then put us back in our room and we’d lay in that bed all day. Well, I’m real stubborn and pigheaded. And I thought to myself, I’m gonna be here six weeks, and that’s what they were telling me six weeks. And I said, I looked around and those people had been there for a long time. And I said no, this is not going to work for me. So my daughter told me and because she thought she could make me believe anything because she was in the medical field. She said Mom, if you check yourself out, they’re not going to your insurance will not pay your medical bills. So okay, so when she left up to my purse, I called my insurance company and I said If I’ve checked myself out, will you pay my medical bills? And they said, Well, of course, what is your plan of action and I told them, I said, a very good friend of mine. I’m he’s a physical therapy. Feel physical therapist, he owns a rehab center. I’ve already spoken with him. My sisters come in Blind him from Houston. She’s gonna take me every day, I will walk faster. And they said, Well, do you have a plan? there and you think it will work for you then? Yeah, so I called down to the nurse’s station, tell them I forget the paperwork ready and check it out. And I call my head. That’s it. Come get me. And I check myself out. And what’s the following week I was up on a walker walking all around my house. And I wouldn’t have been if I had stayed there not do I recommend that for everybody? No. But I knew what I needed. Because mobility is one of the most important thing. And so that’s another reason I don’t like sedation. Because if you’re sedated, and on meds, you’re not gonna be able to get up walk.
Kali Dayton
Right? It makes me wonder if you hadn’t been sedated for those first six days. And you’ve been walking right away if you would not have gotten so behind.
Susan East
Exactly. That’s the problem and say, in 2014, I didn’t have that problem, because I was not sedated. Now, in 2017. It was a different situation, because I had left my home and drove three states away to meet my daughter and her husband at a beach house. And I’d only been there six hours. And she found me unresponsive in my room. And I had to be airlifted to a hospital. And I was in a real coma for seven or nine day so I couldn’t get up. Yeah. So I had the mobility problem there to back. I got myself up and got I got myself walking right away. But as soon as I got out of that coma, and I could get up, I made them get me out. You know, that was your request, necessarily protocol for my role. Because for one, I didn’t want my lungs to get pneumonia. You know, I had meningitis and I was in arts again. So I knew I had to, and I’ve been dented twice at that hospital. So when I got the event the second time, I called him I said I have to get up. I have to get up out of his bed and walk. You know, walking is the best thing to prevent me from getting pneumonia again. Yes. And I have to walk. Sit down care. So myself on ventilator they should be walking. There’s a way?
Kali Dayton
Yes. Yes.
Susan East
You know, you have to do that you have to warm up. And that’s America got just had a back surgery November 18. And the doctors were freaking out because only have 38% total lung capacity left. And it was one of those situations where I had to have this surgery. And so the team was all working to get me prepared. And I told him, I said y’all do your thing that the one thing you better have on hand is the physical therapist where you get me up out of the bed that day, involve me. Because that’s most important to me. I want to walk. I want to walk because you have to the mobility, the mobility, and not being sedated not taking a lot of medications, not a fit, no more thing pack, no, none of that stuff. You know, you can’t do it. You can’t do it, inhale.
Kali Dayton
It sounds like your independence is really important to you.
Susan East
It’s very important to me, because I know that if I don’t if I don’t take care of my medical plan, and I don’t ever see my getting better. Nobody knows how I really feel. Right. That’s your body now. It’s my body. Yes.
Kali Dayton
Did you have to go to rehab? Other times you had arts?
Susan East
No. I did. Well, I did. But I did it. You know, like when I got home from Alabama. I did it. I had some they had someone come to my home and rehab me. And of course, you know, I walk in I keep myself in good shape. And then I know what to do. And like when I would lay in a hospital bed, I would work my legs and work my steps and because I was so careful. I didn’t want like I didn’t want my feet to fall or feet or fall flat if you’re not careful. If you’re laying there too long. And you know, I would lift my legs up and you know, it’s just luckily I knew a lot of the things to do.
Kali Dayton
Because I was burying stuff first time
Susan East
Yes. And because of my daughter and my son in law being ICU nurses, they knew a lot of things to help me with. But that’s why I advocate and try to help so many people. Because I know that these things are so important. And they don’t get told that, you know, nurses don’t have time to sit and do all this right. And we don’t have it.
Kali Dayton
Right. And we have some some barriers, barriers with sedation still. So it’s sometimes it’s hard for us to believe, let alone incorporate the fact that someone can and should be awake while on the ventilator.
Susan East
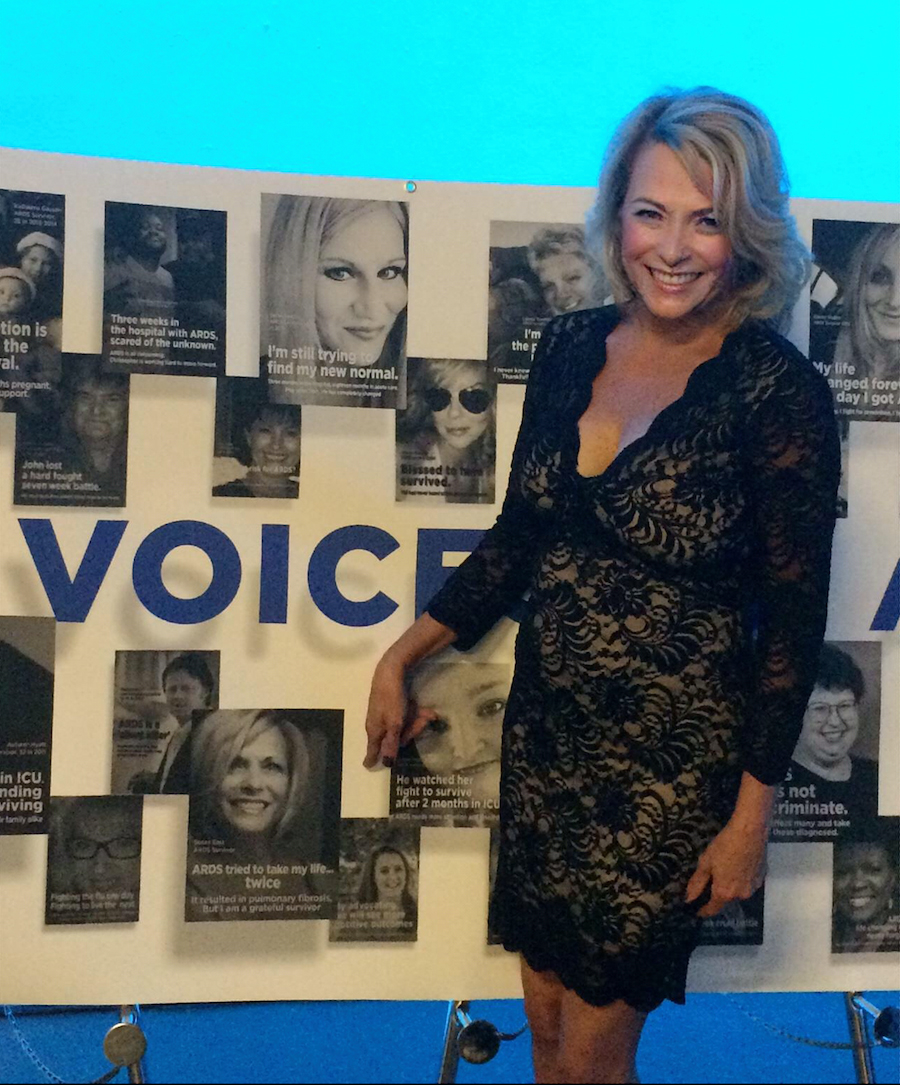
By night, I had pictures of me that I have posted on Facebook, trying to show people where I immobile I was, I didn’t even know they took it. I was sitting there on the ventilator, I come out of my coma, probably the day before I was sitting down there looking at Facebook or something and just as normal as can be, you know, but what’s
Kali Dayton
what? Snag those pictures and post them on our blog so that I listen? I think a lot of people haven’t seen what it looks like to be awake on the ventilator. So it would be really useful, I think.
Susan East
Yeah, because it. You know, I think a lot of it is you had to get positive mentally. You’re gonna overcome it. And there’s a lot of people I talk to on this private message boards, you know, they’re like, Well, I’m scared, I’ll get it twice. I’m like, Well, I’ve had it three times, and it’s okay. You can do it. Yeah. Not saying you will get it a second time. But it happens, you will do it. You can do it.
Kali Dayton
And how did you go about making that declaration that you do not want sedation? Is that part of your directives?
Susan East
Yes. It’s in my it’s in my I had my attorney draw that. Oh, wow. It’s in my in my head, my I went to my attorney and had it drawn up that way.
Kali Dayton
Now, that’s, that’s impressive. And I, I would declare the same thing, even though I haven’t ever been on a ventilator. But I’ve seen the variation in outcomes. And that’s what I want what I would want for myself, but it’s so much more powerful coming from someone that has had it both ways. How’s your life now, after three rounds of art.
Susan East
Even the life of scared arts does not scare me. When I had this surgery, November, there was a 50% chance I was not going to live because of my lungs. And there was a very good chance I was going to have art. I was not afraid. I’m not afraid of it. If I get it, I get it. If I get it, I’ll deal with it. And I’ll overcome it.
Kali Dayton
As long as you’re not sedated.
Susan East
As long as I’m not today, if today, I have no control over it. I can overcome it, if I can find it. But if I’m not awake to find it, I can’t do anything about it. I like it. I totally agree. I have to find it. I’m the only one that can do it.
Kali Dayton
Yeah. Forget that patient. I think we forget that patients can and should participate in the fight in the journey.
Susan East
Yes, they have to. They have to and you have to make them understand they’re strong enough to do this, they can do this. There’s nothing to be afraid of. It’s just a tube.
Kali Dayton
I mean, it’s an uncomfortable tube. And it’s a scary situation. But I see with my patients that if we don’t make them confused with the sedation, and then our cortex and the benzodiazepines. That’s it, they can really have clear brains and cope with it and participate and express themselves and make decisions. So it’s really refreshing to hear that because that’s what I felt when I care for patients is that that’s what is right for patients. So hearing it from you just at home and encouraging
Susan East
them to journal their journey helps and is journaling journey if they can, you know, it helped from being clear headed for one help, because when you’re sedated, I just don’t think that anybody can think straight. First of all, when you’re sedated, it’s your masking whatever’s wrong. For one, it’s not really helping. And, you know, you can’t think straight, you can’t think logically about the situation you’re in and that’s just gonna make it worse. You know, it clear headed, you can stop and rationalize and think, you know, I have panic attacks. You know, I have PTSD, but I can deal with it. Because I can rationalize and stop and think about the situation. And you know how I want my life to be. I’m not gonna let that control me. I’m going to control it.
Kali Dayton
But if you’re sedated, those tools are taken away from you. Yeah,
Susan East
absolutely. I have no control. So great.
Kali Dayton
So, Susan, you’re spot on? Are you? Were you working before? Are you working? Again? What is your functionality like,
Susan East
we have, we own our own business. And just now I mean, I’m I do the accounting work, and I don’t go in there now, as much I do a lot of it from home. But I’m getting to where I’m going back a little bit more time. It’s taken me a while, you know, to get back to going over there and stuff. You know, I just, I don’t know why I just haven’t lost its energy. You know, I’m tired a lot. And I have three grandbabies. Now. So that’s a lot of it too.
Kali Dayton
Which is a good reason.
Susan East
Yes, very good reason. That, you know, I’m a bet. And to volunteer a lot. I like to, you know, I’m very active with doing stuff with art and other things locally, in my community to help out and that’s very important to me to give back. Because I feel like God, I’ve been very fortunate. And, you know, I just want to help and give back to others.
Kali Dayton
I love it. Well, I feel like your testimonial is an incredible contribution to the discussion that we’re having. What would you say to ICU providers caring for patients on ventilators?
Susan East
I’m sorry, what was that?
Kali Dayton
What would you what would you say to ICU providers caring for patients that are on ventilators?
Susan East
I would say if you’re you know, caring for patients on ventilators try and treat them as normal as possible, make them feel as normal as possible, because they need to feel like that machine is no different than an IV or anything else, honestly, you know, people fear on days, but they don’t need to people fear giving blood they don’t need to, you know, especially when you are once you have been on an IV, I mean event or you’ve had art, you’re going to have other issues come up. It’s just a part of your life, you know, or I have, and I just try to think of everything I just like, it’s just a part of my life. And I don’t think of anything as you know, scary or bad, I just kind of laugh at it and go with it. That’s my life now, and I’m just lucky, I have a life. You know, and everybody needs to be nobody needs to be afraid of these machine. These machines are saving our lives. It’s just like, when I was moved in LA, I was moved to put on ECMO. And I was mentally prepared for ECMO. You just, you know, you have to, you know, these machines, you know, some people are like nail you may have to be put on a band. Now, if you’re gonna be combat you’re high you’re gonna be might be put on the stand. It’s gonna save your life. But you know what? You knew this? You know what I mean? Yeah. Mind over matter. Hmm. Good, positive pastored.
Kali Dayton
I like it. And I think one of the concerns as ICU providers is that if patients are awake, they’ll pull their to bout. But what you’re saying and what I seen is that when we allow them to be awake, and understand and clear headed, that they understand that to this keeping them alive, and they
Susan East
pretend it never once tugged at my tube ever. Right? Because it wasn’t brighter, but I knew what it was there for.
Kali Dayton
Right? Because you weren’t confused anymore? No,
Susan East
there was no confusion. None. Well, this is yeah, when I was when I was medically sedated at that one hospital. And that was a very bad experience. I can remember when the very first time they put me in a chair when I bought me out of it and they put me in a chair to feed me. And this was horrible. They put that tray in front of me. And I thought okay, you know, because I really couldn’t comprehend what was going on. Because I was drugged. I was just druggie. And I said, Feed yourself. And I was like, I can’t. I said, Yes, you can. And I literally couldn’t. And I felt like I was being shamed because I couldn’t get that spoon or fork or whatever to my mouth. And, you know, I think that was the worst thing in the world but the best for me because it made me realize I will never depend on me again. But by not doing that means I cannot get in that mental state. They can’t drug me like that again. If That’s why I couldn’t do it.
Kali Dayton
Right. I love it. And I think more patients would have your, your fighting spirit if we allowed them to.
Susan East
Yes, absolutely, I think so to a really good people are stronger than they realize when they have to be that can do it, they can really do it. But if we weaken
Kali Dayton
them with days of delirium, then then we take away their their capacities to cope and to work.
Susan East
And then they stand a risk of getting, you know, dependent on something or thinking I need it, and I don’t that’s why we have such an addiction problem in our world today.
Kali Dayton
Yep. And it kind of starts with those first moments and the ICU. It does. Well, Susan, thank you so much. This has been so helpful.
Susan East
Well, you’re so welcome. And I’m going to email you those pictures and you’re more than welcome to use them. However, you know, whatever I can do to help. I’m here to help.
Kali Dayton
Thank you. You’re such a great use resource. We’ll keep using you. We’ll come back.
Susan East
Absolutely. Okay.
Kali Dayton
Thank you then.
Susan East
Thank you.

Transcribed by https://otter.ai
SUBSCRIBE TO THE PODCAST




