SUBSCRIBE TO THE PODCAST
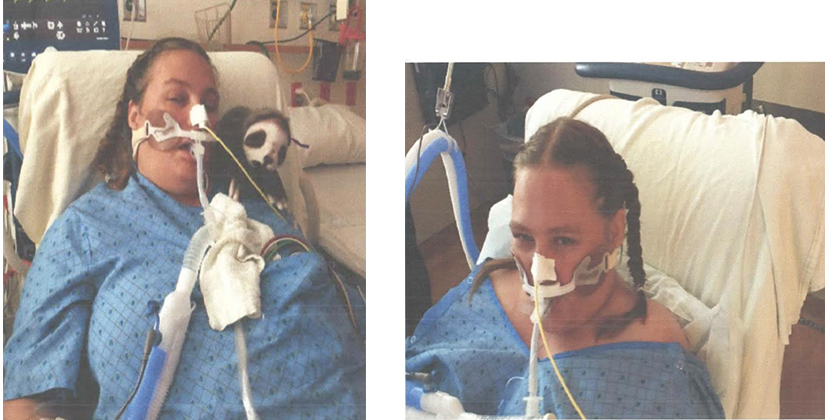
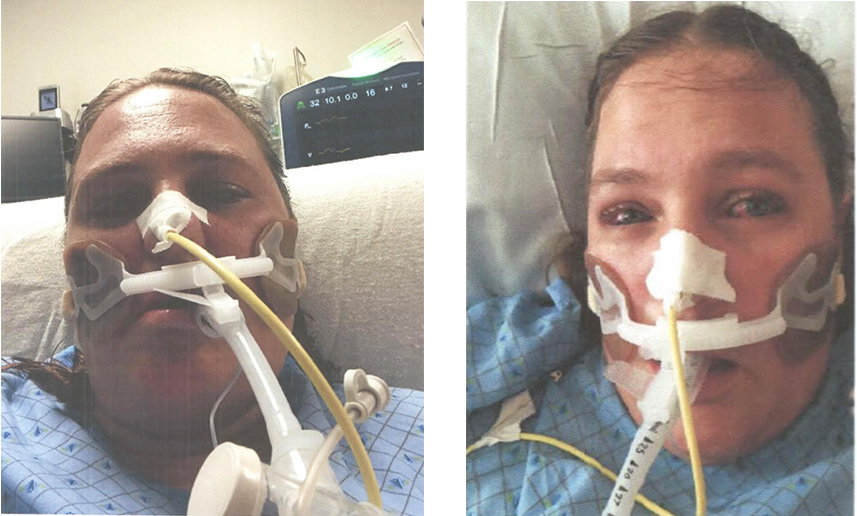
Joan Johnston was admitted for ARDS and remained on the ventilator for 17 days. Here, she shares with us what it was like to be awake, walking, and even showering while intubated.
Episode Transcription
Kali Dayton
Hello, and welcome back. Today we’re going to be talking to Joan Johnston. She was a 38 year old that was admitted to the ICU in September of 2018 for mild ARDS. When she was initially intubated, she was requiring an Fi02 of 100% and Peep of 16. Eventually she weaned down to but was stuck on a PEEP of 12 and Fi02 50%.
She was intubated for 17 days. Fortunately for her, she was awake and walking the whole time. By the time she left the ICU. She was walking over 1000 feet. She walked straight out of the hospital doors, and went right home. She’s with us today to tell us what it was like to be awake and walking on the ventilator. Joanne, thanks so much for joining us. So tell us about your ARDS journey.
Joan Johnston
Um, my ARDS. I started I was admitted into the hospital here in in my hometown, on September 20. Two days later, I was life-flighted and was in the ICU for 17 days. intubated.
So yeah, I woke up that morning feeling just fine. By the end of the day, I was in a blackout in my bed with a blanket over me. And I was freezing cold in the emergency room and my saturation. My oxygen saturation was below 72. And so I was given oxygen and admitted to the hospital with pneumonia. Yeah. Then two days later, I was completely. The doctors here were baffled. They didn’t know what was going on as to why I was on 100%. I needed oxygen completely. My lungs were pretty much shut down. And so yeah, I was life flighted. And then spent 17 days intubated and awake
Kali Dayton
You were awake the whole time?
Joan Johnston
As far as I know, yes. The whole time. I remember being awake, through all of it.
Kali Dayton
And what was it like to be awake on the ventilator?
Joan Johnston
Horrible. It was horrible. I gagged constantly.
Kali Dayton
You did have the strongest gag I’ve ever seen. Most people do not have as hard of time as you did. But you must have had a really strong gag reflex. And then for some reason, the tube would move out a little bit. And that would just trigger you. So I do remember that you. You were exceptionally uncomfortable. Most people really are calm on the ventilator. But you had this terrible gag and even still, you stayed calm.
Joan Johnston
Yeah, I use that. I think it was just the will to to survive. To thrive. You know, I had realized that, you know, “I’m not getting out of here unless I do something about it.”
Kali Dayton
You know, I asked you, if you would have rather been sedated at that moment. And you told me now, do you still say that? how come?
Joan Johnston
Because I think that I mean, I was able to converse with my doctor and, and even though my doctor, when I would ask him, you know, am I gonna die? He never really gave me a straight answer.
But at least I was getting answers. In on every time any of the doctors came in any of the nurses were always up front when he told me what they were doing at all times. And so that was so much it was easier for me to know that I think if I would have been asleep and I went through the- what is called-ICU delirium at the very beginning. –If I had to go through that for 17 days, I think I would have been…. you would have to put me in a loony bin.
Kali Dayton
So tell me a little bit more about that. I think your life flighted, right? You were intubated elsewhere, and likely started on sedation right after you were intubated, and then likely stayed on sedation while you were with life-flight. And I know that once you came to this hospital, sedation was taken off. That was probably, I don’t know… 12 plus hours of sedation. What was that like for you?
Joan Johnston
That was a horrible. I thought all nurses were teenagers. At one point in time, they were… I can’t remember what kind of tests they were doing. But they were going right through the artery in my wrist. Yeah, and it feels like…you’ve taken a little tiny saw.
He was just… sawing into my, into my wrist. So the, the nurse I had looked like a teenage boy. And he kept telling me I’m so sorry. I’m so sorry. And I could have swore he was sawing my wrist off.
Kali Dayton
And did you know what he was doing? Could you comprehend or cope with it?
Joan Johnston
No, I didn’t know what he was doing. At that time, I, there was so many people around me, and they’re telling me to calm down and I’m going “Calm down!? Are you kidding me? You got me chained down?”- At that time, I was handcuffed to the bed.
Kali Dayton
And then, so you were probably restrained, right? You had your hands tied down?
Joan Johnston
Because I was trying to take the tube out.
Kali Dayton
Because nothing made sense. Correct?
Joan Johnston
Yeah.
Kali Dayton
And then when you came here, and you the sedation was taken off, and you were woken up, and everything was explained to you and clear, you never had restraints on? Correct?
Joan Johnston
Correct.
Kali Dayton
That’s great. I remember you doing homework with your daughters in the room!
Joan Johnston
I did. My my daughters were very… it scared them. And I don’t think I would have one wanted my kids there.
Kali Dayton
How old are they?
Joan Johnston
My daughter, my oldest is 19. And my youngest is 13. But at the time there was they were 17 and 11.
Kali Dayton
What did it mean to them to be able to interact with you during that scary time?
Joan Johnston
Like I said that they were terrified during that time, I think. But they were so glad to see me too, because they hadn’t seen me for a couple of days.
And I say that, that I wouldn’t want them to be there. But at the same time, I hope thatthey don’t pick up a cigarette like I know I did in the past.
Kali Dayton
Right.
Joan Johnston
Ya know, I hope they learn from my experience seeing the pain that I went through.
Kali Dayton
How do you think the the stress level or the emotional trauma would have been for them if you’d been sedated during that time? What difference does that make to them? Do you surmise?
Joan Johnston
HUGE. Huge. My youngest was very, very attached to my hip. And so not have me there and not to be able to interact with me… I think it would have been detrimental to her. But to be able to be there with me even, though she, you know, she was scared to come up to me.. I think that that would have been detrimental to her.
Kali Dayton
And you were helping her with homework. It was awesome.
Joan Johnston
Yeah.
Kali Dayton
And though you were confused a little bit at the beginning… Once you cleared out, you stayed clear the whole time.
Joan Johnston
Correct.
Kali Dayton
You were sleeping at night and awake during the day and aware of everything?
Joan Johnston
Yes.
Kali Dayton
Yeah, you were, I’m looking back at your records, you were pretty sick. You were required to peep of 16 though An oxygen requirement 50%. But a peep of 16 is is quite a bit of pressure. So you had some mild ARDS, you never had to be proned, like laid down face down, like some with ARDS do. But you still really required a lot of support from the ventilator. And so you were intubated for how many days?
Joan Johnston
17 days.
Kali Dayton
17 days. And, you know, when we talk about time or length of time being intubated, it’s a little bit different. It’s almost comparing apples and oranges. Because when someone is awake and walking them until later, they… statistics show that they get the tube out faster. So even though you were still awake and walking… your lungs were so sick, that you still had to have the tube in for 17 days.
Joan Johnston
Right.
Kali Dayton
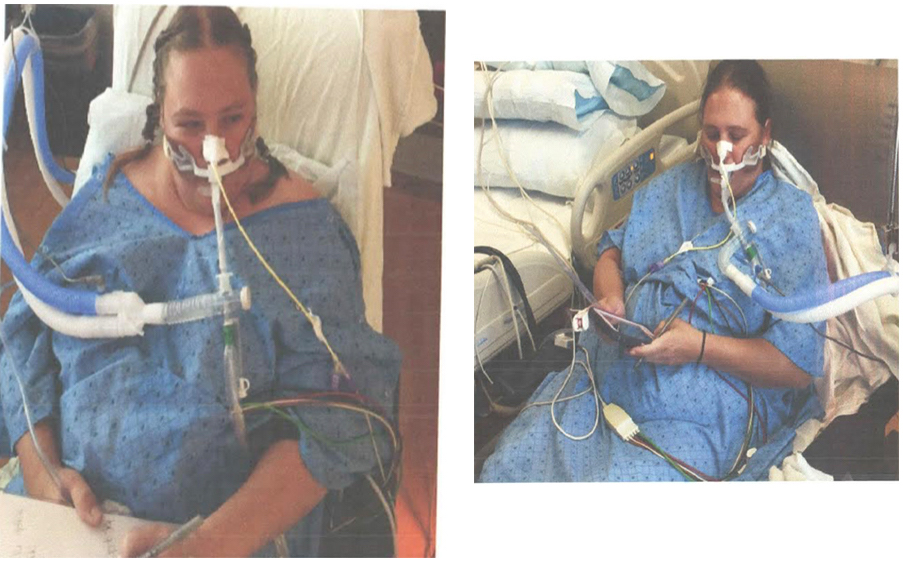
So sometimes we think that if someone is able to get up awake, be awake and walking, that they’re not actually that sick, or that we should take the tube out. But according to your ventilator support requirements, you were still really dependent on the ventilator and yet you were awake and walking. What did that mean to you? Or what was that like to walk on the ventilator?
Joan Johnston
To walk on the ventilator because of my gag was was horrible, but they kept… my nurses and everybody just kept pushing me and said if you want to get better you want to get out of this out of the ICU .. you’ve got to get up and walk. So to be able to get up… it’s huge.
You know, I most of the ARDS patients… I can’t relate to because I wasn’t sedated. I was awake through the whole entire thing. And so it’s huge.
Kali Dayton
That’s how you and I became re-connected right? I had joined an ARD survivor group because I wanted to understand the patient’s perspective. And I asked, you know, there are hundreds of survivors from all over the country in the world – “Who had been awake and walking on the ventilator?” – And one person electronically raised their hand and said, “I was!” – and I got excited. I thought, “who else is doing this?”
And I asked you where you had would been? And you said, the name of the hospital, and I realized that- I knew you. You had been my patient. And so you asked for me to start a survivor group for this specific ICU because our course of treatment is different, and therefore the outcomes are different.
And so you’re right, a lot of what people are talking about is their, their trauma, their PTSD from the hallucinations, which you can kind of understand because you had that, that day of hallucinations and confusion.
That 17 days straight. And in reality, it probably would have been longer than that. If you’d gotten sedation, you would have been intubated for longer, likely would have had that delirium for much longer, even after the tube was out.
And so what does it mean to you to know that your your treatment was different, your course is different, and your outcome was different, that you you got the tube out faster and walked out of the hospital and went home?
What does that what does that mean to you be able to walk out of the out of the ICU and not have to go right into a treatment center to learn to walk, talk and everything?
Joan Johnston
It was so rewarding. And I give total credit for my whole entire recovery to my Lord and Savior, because I probably wouldn’t made it. You know, this is just amazing that I was able to just walk out, you know, walk love it.
Kali Dayton
And you worked hard, you did your part. You know, you were walking, what 200 – 400 feet multiple laps around the ICU at least three times a day. I think that that played a huge role in your preservation of function, being able to walk out the ICU and go home.
I have a picture of your ventilator outside in the hall while you’re in the shower room. So you were showered while on the ventilator. And most people won’t even believe that that’s possible.
So can you tell us what that was? Like? What did that mean to you to be able to take a shower, even on the ventilator for 17 days?
Joan Johnston
The very first time was very unpleasant. They had told me that if if I wasn’t able to get a shower or something that they wouldn’t tell my hair.
So my nurse that night that I think was a very first night I don’t know. The very first shower was horrible, again, through the whole entire thing.
But after after that my showers got easier and easier. And once I started being able to wash myself… Because before then when I ran the shower, somebody else had to do it for me. But once I was able to wash myself, yeah, when I was able to wash myself where there was there was a nurse outside the door.
Kali Dayton
Even on the ventilator!
Joan Johnston
Yeah, that’s pretty amazing.
Kali Dayton
Yeah, I think if you hadn’t moved that whole time, if you had been said, sedated and immobile. There’s no way you’d walk yourself to the shower like you did, let alone be able to safely stand in the shower. But even intubated with extension to into the ventilator. You were able to stand with a peep of 16 or 12, whatever you were on at the time. And even have that dignity of being able to wash yourself. That’s amazing.
Joan Johnston
Yeah, that was probably my favorite part.
Kali Dayton
Yeah, I.. I can’t imagine going to 17 plus days without a shower.
Joan Johnston
Yeah,
Kali Dayton
That would be so hard. Um, so you went straight home after the ICU, and 46 to 80% of survivors have cognitive deficits. Sorry, 46 80% of ARDS survivors have cognitive deficits a year after discharge, and now you’re past a year after discharge. Do you have any cognitive deficits?
Joan Johnston
I don’t. I don’t, nope.
Kali Dayton
Did you go back to work?
Joan Johnston
I did go back to work I went to I went back to work probably five months, maybe not even that. Probably sooner than that because I co-own my own business. So I kind of was pushed right back in I was doing it at Home part time, and then, you know, coming in when I could.
So yeah, I went to work pretty quick.
Kali Dayton
Do you feel like you’re able to keep up like you were before?
Joan Johnston
For the first year, it was really, really, really difficult. But yeah, since this year, you know, I haven’t had to be on oxygen for almost five months.
Kali Dayton
That’s great. Congratulations.
Joan Johnston
Yeah. Yeah, for the first year, I was out, I was on oxygen a lot at work and everything. So yeah.
Kali Dayton
There are lots of elements to the recovery process after the ICU. A third of survivors of ICU survivors in general, cannot go back to work 60 months after discharge?
What does it mean to you to be able to work and have the career that you were doing before?
Joan Johnston
Very, very rewarding, because I could have lost it all. You know, however, what I’m 40. And to realize that I wouldn’t be able to, if I didn’t have the job I have now I wouldn’t been able to, there’s nobody that’s gonna hire somebody that needs to be on oxygen.
If you have to say, “I’m sorry, I’m a little bit breathless today”, or “I came down with a cold and I need to be really cautious” or ya know. So it’s huge, to be able to go back to work, and all night, and I didn’t have what I’ve, I’ve heard other other ARDS patients where they say, “I’m losing my house and everything”. I was so blessed, to come back to work soon.
Kali Dayton
I love hearing that. That truly is what this is about – is not just saving a life but preserving it.
And a lot of our survivors struggle with quality of life afterwards. How is your quality of life even little after a year of post discharge?
Joan Johnston
A little bit problems with my lungs, mainly in higher elevations, when there’s a lot of moisture in the air. But like I said, I don’t require the oxygen is much my oxygen saturation doesn’t ever go above 95. But usually, when it goes below 90, that’s when I start getting lightheaded.
And so my quality of life is I have an abundance of life, you know, as compared to others, you know? Yeah. Others that have been in my situation. And yeah, so being awake, being awake is so rewarding. I would not change it for anything, as much as the pain. It was the worst pain I’d ever went through. It was the worst nightmare I’d ever went through. But I wouldn’t change it. I’d still want to be awake again.
Kali Dayton
That is so good to hear. I’ve been called “unethical”, “inhumane”.. all the things from other health care professionals that don’t quite understand what it’s really like for patients. So I am so grateful that you’re willing to come on and share with us your perspective and insights. And I’m glad you’re doing so well. You’ve worked hard for these outcomes and you deserve them.
Transcribed by https://otter.ai
SUBSCRIBE TO THE PODCAST




