SUBSCRIBE TO THE PODCAST
When 69-year-old Dr. Ken Hurwitz was intubated for COVID19, how was his life saved and even preserved? After 3 weeks on the ventilator, why was he able to walk away and go straight home?
Episode Transcription
Kali Dayton 0:28
In the past few episodes, we learned about the conditions, treatments and outcomes experienced during the COVID 19 pandemic in New York, we recognize the dire circumstances in which these heroic providers were relentlessly working and the desperate measures required.
I have received many inquiries about the status care and outcomes for COVID-19 patients in the awake and walking ICU. Later, I will have my expert colleagues share their approaches to the difficult changes the critical care world faces. Yet as always, we will first address these questions with our why with us this episode is Dr. Kenneth Hurwitz, one of our first COVID-19 patients with his wife Beverly to share with us their journey, care and outcomes from the awake and walking ICU.
Dr. Kenneth Hurwitz 1:17
Hi, my name is Kenneth Hurwitz. I’m now 70 years old. I’m a retired pediatrician and regenerative medicine doctor in hospital for 28 days with COVID.
Kali Dayton 1:34
And Beverly, can you tell us a little bit about yourself,
Dr. Beverly Hurwitz 1:37
Hello, I’m Beverly Hurwitz, I’m 72 years old. I am also a retired physician. And my initial training was in pediatrics, and I had subspecialty training in neurology and had a varied career thereafter.
Kali Dayton 2:01
So talk a little bit about your COVID journey.
Dr. Kenneth Hurwitz 2:07
I contracted COVID, somewhere, maybe in an airport, maybe in a restaurant, I don’t really know. And gone to a wedding in Arizona, where there was 150 people about a week or so before I contracted COVID. But nobody at that whole wedding was affected. So I assumed that I had attracted at somewhere in the airport coming home from Phoenix. And we Beverly and I both had the COVID at the same time. So I had about 13 days at home. And then my memory of being home with the viruses really vague. I just remember the last day when I had to be admitted to the hospital. And that was on the night or the afternoon of March 26.
And then I remember being wheeled into the emergency room saying hello to one of the nurses waving. And that’s the last day remember, I know I was airlifted to I don’t we call anything until I think April 11 or April 12. Even though I had ups and downs in the hospital, I know I was conscious for some of that time period and then sedated and put into facedown position in a coma for eight days. But I don’t recall anything during those during that time. I had lots of different dreams. And maybe some of those dreams occurred during that period. And I can’t be sure. And I know a lot of dreams after April 11 When I think I woke up and no longer needed to be sedated, heavily sedated or put down in the prone position.
Kali Dayton 3:58
And I am so fascinated to hear that because we watched you spent a few days at the outset hospital on nasal cannula. And this is the beginning of the COVID wave. When we started intubating everyone that required more than six liters, nasal cannula. So as soon as you required more than six liters, you were intubated there and then flown to our hospital. And I think you were sedated for transportation. And then once you came to us we took off the sedation and you woke up and you were you were pretty with it. You were writing notes on the board on boards.
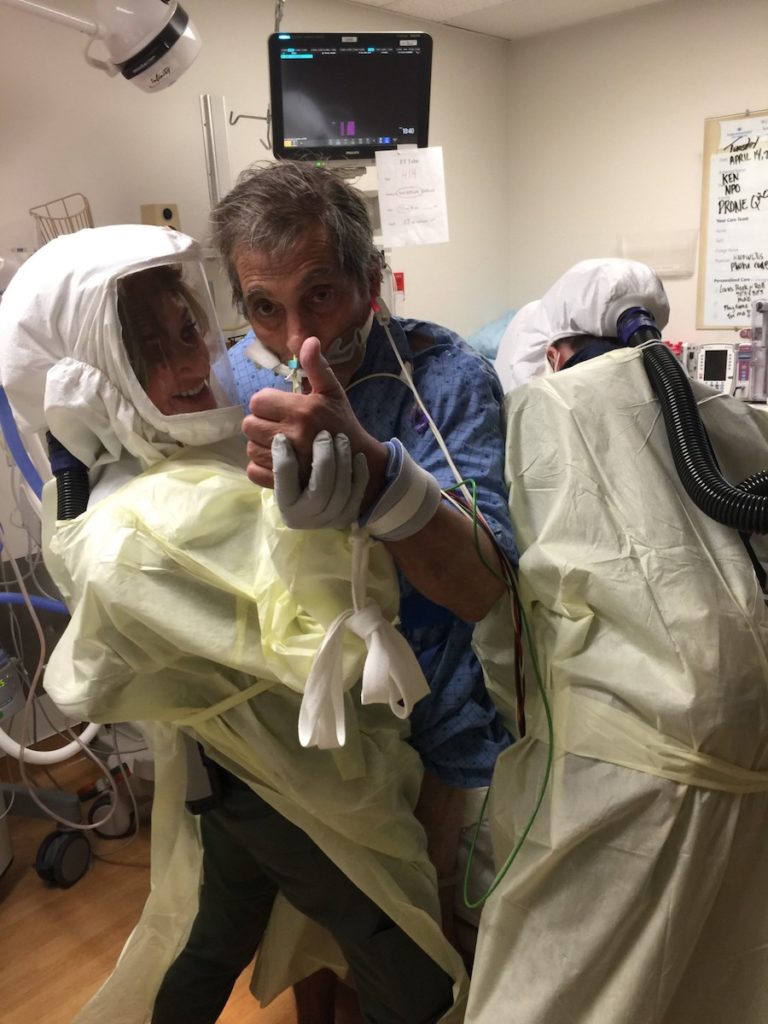
You were making very specific requests such as you want to atropine drops because your mouth was really moist, you want to albuterol you knew what you wanted. It was a little bit frustrating because you didn’t have your phone with you. And I really felt like maybe that would help you be able to talk to Beverly during that time. This is all just new to us, I mean, having to wear the PAPRS and being isolated in the room.
And yet, during those six first days with us on the ventilator, you were CAM negative, meaning you would answer questions very appropriately, you could follow pay attention. You seemed really with it. You were pretty anxious. And Beverly and I would talk this whole time how this virus seems to be so neurotoxic. And that’s something that we’re noticing in critical care world, that even when people aren’t sedated, they’re becoming delirious. They’re, their brains aren’t the same. So what you’re saying is that, even though you were responding, so appropriately, you weren’t quite yourself, and you don’t recall, I don’t recall that.
Dr. Kenneth Hurwitz 5:50
No,
Kali Dayton 5:50
You were even walking in your room with physical therapy. So you know, they were just making it up as they went. Because it’s so new. Usually, we have people walking circles around the ICU. But that wasn’t an option. Since now, we’re in negative pressure rooms and an isolation. And so we had to walk into the door, we lean back walking to the door, we lean back, we had to use an arm bike. They took stools when they are because or was shut down. And you were stepping on the stools.
And do whatever we could to keep your brain and your body going. And you were doing really well except for anxiety, we could tell you were so anxious. And we wish that Beverly could have been there because I think that would have helped. So that was one of some of our challenges starting with COVID. With you, but you were doing so well. And you were on pretty minimal ventilator settings.
Dr. Kenneth Hurwitz 6:48
Wow.
Kali Dayton 6:49
And then after six days, your lungs started getting worse. And so we proned you, so you’re laying on your stomach, and that just wasn’t comfortable. So we started some light sedation like precedex and fentanyl. You were still able to help turn, you were still asking questions, you were writing on the board. And the interesting thing that I found is, a lot of times with ARDS, oxygen consumption is such a problem by that point. If someone coughs, they have no reserve, their oxygen plummets.
You couldn’t be supine, or your oxygen would drop. And yet you could basically do a push up in the bed, and your oxygen wouldn’t drop as long as you were facedown. So you were helping turn yourself. You were doing push ups. Just repositioning yourself but still the same kind of motion which I would have expected your oxygen to drop and yet it didn’t.
So you were on very light sedation, pretty awake pretty with it answered yes or no can they get it for two days. And then your lungs got even worse. So then we felt like we needed to paralyze you. And so we put you under deep sedation and paralytics for two days. And even after we took off the paralytics when we tried to take off the sedation, at that point, oxygen consumption was a problem. If you moved, your oxygen would drop. So we had to keep you more deeply sedated. So you were sedated for total of six days prone for a total of eight days.
When your oxygen got better, so every day we were trying to flip you trying to see if you could be on your back again. You’d be okay for more extended amounts of time and one day once we noticed that you really could handle the being been on your back and we took the sedation completely off and you were okay. It was actually a nurse and a respiratory therapist. I don’t think physical therapy was even there. It was our nurse Patty, who is very dedicated to the mobility, the big picture care of patients. She said, “Okay, he’s been down long enough. Let’s get him up.” So after eight days, of being on your face not moving. Patty and a respiratory therapist set you up.
Dr. Kenneth Hurwitz 9:10
And like April 11,,
Kali Dayton 9:14
probably
Dr. Kenneth Hurwitz 9:15
I have pictures on my phone that the nurses took. And that’s the only reason why I would know that thing. So that’s probably what it was. That’s what I think I was really big became conscious that all those other episodes you were talking about. I don’t recall those as well.
Kali Dayton 9:39
And that’s so interesting, because yeah, a lot of people are able to remember their hospitalization and their time the ventilator very vividly. But despite our best efforts to keep you clear you, you still were neurologically affected by the virus. And you said that you were having weird dreams and hallucinations. Can you tell us more about what that was like?
Dr. Kenneth Hurwitz 10:00
While I had these dreams that actually would carry on, not still dreaming. But the next day when I woke up, they would seem like those events really happened. And for instance, I had a dream about one of our dear friends, who was trying to make me a better golfer by giving me oxygen, oxygen added with something else. And during this experience of him having me in bed, there was a whole group of other people there. And they’re actually giving me the COVID virus.
That’s, that’s what that’s what was happening. And, of course, I was restrained. I couldn’t talk. I couldn’t say anything. So it was very, very frustrating. And had these dreams about three times. And the last time I had it, I said, when I wake up… I didn’t know I was sleeping…. So, “the next day, I’m going to tell Beverly, to stay away from this individual, because he’s a fraud, and he’s a bad person.”
So I was able to write out on a board, “Beverly, please stay away from what’s his name, he’s a fraud.”- And it was so real, that I couldn’t separate dreams from reality. I couldn’t separate it. And had a couple like that were other other experiences where I couldn’t tell if my dream and my reality I couldn’t separate reality from my dreams.
Kali Dayton 11:32
And so the stress of those, those scenarios in your mind was just as vivid as if it was actually happening.
Dr. Kenneth Hurwitz 11:42
Yeah, very true. Right.
Dr. Beverly Hurwitz 11:44
Your extubation…
Dr. Kenneth Hurwitz 11:46
my extubation dream, my extra bed in myself. I was in this medieval battle with guys with shields and clubs, despite clubs, torches, and I was fighting this guy about a shield on his face. He had me by the throat and ripped his hand off of my throat, and had pulled my tube out. And that’s…
Kali Dayton 12:11
Oh…You were severely delirious. We knew that you were delirious when we first took sedation off. We were working hard to clear it out. So first, you could only sit at the side of the bed. And then physical therapy, even that afternoon was like, “let’s try standing”.
And then over the following days, you were starting to stand and walk again in the room. Just even just little steps. You were extremely weak. But you were extremely delirious, too. And we were worried about that. And so we had you restrained. And somehow, you did…. you use shimmied down and you got to ahold of that tube. And when they came in…. And by that time, your lungs were getting better. And you really were strong. You could clear your secretions. You could take your own breaths. So when they came in, you said, “Oh, I didn’t need it anymore.”
Dr. Kenneth Hurwitz 13:02
Oh,
Kali Dayton 13:03
and you weren’t wrong! It made us laugh. We thought, well, he’s also a physician. He knew he didn’t need it. We didn’t know you were hallucinating though.
Dr. Kenneth Hurwitz 13:11
That’s not fun having a tube in your throat for 20 days, or whatever it was?
Kali Dayton 13:16
No, no. And I think if you hadn’t been moving prior to be pronned…. let’s say if you had come in to maybe a different hospital, different ICU and you were immediately deeply sedated….. those six days that you spent walking, and being awake on the ventilator, would have been wasting away. You know, you would have been losing a lot of muscle. And then your lungs got worse. And so we had to prone you. And then we had to paralyze and sedate and do all those things. But you would have already started that that treatment, very deconditioned.
And then you would have been continued to have been deeply sedated even after you could be supine, because that’s just what we do when someone is on a ventilator. But fortunately, you were awake. And yes, you did self-extubate. So a lot of the concern of critical care world is: “What if they self-extubate?”
But our question is always, “what if they never walk?”
“What if we can’t get them off the ventilator?”
“What do they have to be trached because they’re so weak?”
“What did they spend an extra 20 days on the ventilator because of the weakness that we maybe could have prevented?”
And so no worries, but we had almost, we probably had a little over two years of no self-extubations in in our unit until you broke the record.
Dr. Kenneth Hurwitz 14:37
Okay.
Kali Dayton 14:39
But, but it’s okay. And I think the circumstances are so hard. I think that under normal circumstances, Beverly could have been there. We could have been at the bedside more. There was a lot that contributed to that circumstance. And yet, even with the A to F bundle shows that incidences like self extubation happened just as much if not more without deep sedation, and yet, people pass. Meaning they don’t have to be re-intubated.
So when people are deeply sedated, they can still self-extubate, but then they’re so weak, that they’re more risk of having to be re-intubated. So when you said I don’t need it anymore, you weren’t wrong. We just put you on a high flow nasal cannula. And you did great. So, I mean, you probably could have died by self-extubating yourself if you hadn’t been mobilized if you hadn’t been awake and having had spent four days rehabilitating already from being proned.
Dr. Kenneth Hurwitz 15:37
Right.
Kali Dayton 15:38
And so after this four days, you were right, you self-extubated, and you were done with it. We had you on high flow. And yet you were still hallucinating. But you were able to tell us you were telling the staff about things that you were seeing, you said, “I know that Beverly is not in the garbage can. But I see her there. I see a dog, I know the dogs not there.” You were between worlds. How stressful was that for you?
Dr. Kenneth Hurwitz 16:03
Well, I remember seeing like mice, I remember seeing always thinking there was somebody else in my bed or near my bed. When I was I didn’t know that they had put bettadine for some reason on my right knee and it looked kind of yellow. And in some of my dreams. There were these Asian people along with the our friend like golf with was trying to make me a better golfer. He was he was with these Asian people who were doing this therapy.
And when I looked at my knee, it looked like the back of a bald head. And it was like spooked me out. I thought there was somebody in my bed at all times. So and I would realize it was my knee. I mean, it didn’t persist for a long time. But I had these hallucinations of saying things flying by seeing flies like…. flies have kind of fluttered that we’re carrying the virus and we see them every so often. And black, little black specks. I would say I even asked the nurses “Do you see black specks here?” because I’ve ever seen these and I kind of knew that they weren’t real, because they didn’t persist all the time. And so I wasn’t really that concerned about.
Kali Dayton 17:24
So you knew you were at the hospital by that point?
Dr. Kenneth Hurwitz 17:27
Right. And it was in the hospital. I had had trouble. I would say after April 11th, when I think I first remember the nurse coming in the room. I opened my eyes and she had the smiley face that “Good morning, Kenny!”. And it was light and bright. And I thought it was that I woke up that that’s it. I remember.
But I didn’t have any real sense of time. I couldn’t really separate night and day. That was really confusing to me. I think it was one o’clock in the morning. I was one o’clock in the afternoon. And my sleep cycle was way off. So that was kind of confusing. I didn’t of course, I didn’t know the date. They would ask me what the what today is. And I had no reference as I was reading any newspapers. I wasn’t watching TV. So I really didn’t know what day of the week it was or what the date was. So I was confused in that aspect.
Kali Dayton 18:22
And as they started moving you more, you made comments about how weak you were and you were frustrated. Do you remember that? What was it like?
Dr. Kenneth Hurwitz 18:30
Very weak.
Kali Dayton 18:32
What was it like to move again?
Dr. Kenneth Hurwitz 18:34
Well, I knew I had to, but I was a little bit more comfortable lazy in my bed that I knew I had to get up. And one of the pictures I have on my phone is being supported grabbing Angele I think was by the waist and she picked me up and stood me up. And it was very hard for me with my balance and my legs are very weak. And then she had me using like a stationary pedal device to build up my strength. I have pictures and videos of that on my phone. But I knew that was the only way I was getting out of there. So I had to do the PT. I had to force myself to start mobilizing.
And I kind of have to preface because you said that you just turned 70. You were admitted a 69 year old but I have to tell her listeners that you are not a normal 69 year old. Biologically you’re more in your 50s.
You know that you’re probably saved me because I worked out almost every day the gym when I wasn’t doing that. In addition to that I was skiing every day, just about every day. Golf every day we hike every day are very active. And I had no comorbidities no diabetes, hypertension, no heart disease, so I was in good shape. And actually for my birthday, which was a week ago.
My best birthday present was coming off of oxygen. So I was on oxygen for about four and a half weeks. That day, I was able to greet my neighbors out back then have a big celebration for me. And I gave a little spiel and didn’t need oxygen, went out the front of the house, we walked our dog with Beverly, and walked up and down the street. And I’ve only used oxygen in the past for when I was doing my PT. So I wouldn’t drop down below 90. And I’ve been knocked off oxygen Now, last week, drove down to IHC actually drove the car at my echo done in my heart this week and just had a CAT scan, I drove myself to the hospital because I couldn’t go. And so I’m really pretty functional. And actually, yesterday, they played golf.
Kali Dayton 20:43
Wow. What does that mean to you, and just a little context, we’re finding in these overloaded areas, that they are having a really hard time placing people meaning they don’t know what to do with them after their lungs get better, and yet, they’re having to be traped. Still ventilator dependent, still not waking up, or still delirious, can’t hold, pull the finger up. And some of these people are in their 30s 40s 50s. And other. They’re not just elderly that are weak to begin with. These are people that have been immobilized for at least three weeks. And now the ICU is are kind of stuck with them, because there’s no way they can get off the ventilator. Or if they can, there’s no way they can go home. And yet here you are as a 69 year old. If you’d been to a different hospital, you would have been sedated for at least three to four weeks and probably then needed to be on a ventilator for even longer.
Dr. Beverly Hurwitz 21:38
But there it was, wherever they were gonna have a bed for him. I really, I was just lucky to have that choice. Right? We just were fortunate that that’s where he went.
Kali Dayton 21:51
And you are home. You are golfing here with your neighbors you’re walking, you’re taking care of yourself, you at home 10 days after being extubated.
Dr. Kenneth Hurwitz 22:00
Right.
Kali Dayton 22:00
They wheeled you to the front door, you got yourself into the car, I have a video of you getting yourself out of the wheelchair, like like no big deal. You got yourself into the car, shut that door. You all but gave us the finger. I mean, there was no looking back. Right?
Dr. Kenneth Hurwitz 22:12
I love you guys. I mean, I tell I tell everybody had the most loving, affectionate professional care. I mean, I’ve been a physician a long time, I’ve worked in the most primitive hospitals, I’ve been on staff at the most prestigious university hospitals. And I’ve never witnessed or experienced anything. Like the the care that I received was just fantastic. I love everybody there. They their whole purpose in life was to get me out of there. And that’s what got me out of there says Kenny, you’re going to do this, you’re getting up, you’re going to work. We’re getting you out of here. And their ability to get me to do that was so cool. It got me through. I mean, I love you guys, really.
Kali Dayton 23:01
Well you came in such a scary time. I think we… this is such a new virus. New isolation, we were hearing all these really scary stories about how bad it gets. And then we watched you get that bad. And then we’re hearing about 88% mortality rate to people on ventilators. Yet I watched my team, stick to the things that they knew worked. We already had a culture of knowing how to keep people awake and moving. And we knew our “why”. So even when you got so bad, and you had to be immobilized and sedated. We still, once we could, we had you back on course to going in home. And this isn’t a big hospital. It’s not a famous hospital, but it is a strong team with a strong culture. And what does that mean now to your life? Over a month or so later? To be where you’re at?
Dr. Kenneth Hurwitz 23:57
You’re making me cry because I’m so grateful that that you treated me that way. After, after reading your little blurb about what went on with me, and Beverly kept a journal of everything that happened every day. And I hadn’t read that. I kind of avoided that until the other day. And I read that and I said, Wow. I didn’t realize what was going on, and how sick I was. And I’m glad I didn’t know. When I went into the hospital. I think I was under the impression at that time that 97% of the people survive. I didn’t know that 88% on the ventilator didn’t. And I’m glad I didn’t know that. I know. I didn’t want to get intubated when I left. But I’m just so grateful that you treated me this way. And I hope you’re having the same experience with other people or intensive care now.
Kali Dayton 24:52
Yeah, our volumes have increased since then you were one of our first and yet the load has still been manageable. We’ve still been able to keep people awake. And so I just the last day worked, I walked around and I saw multiple people awake, sitting in chairs on the ventilator, all COVID positive, they’re writing notes. You actually were the one that… I was so worried about your ability to communicate. You seemed really frustrated, not able to communicate with us.
Dr. Kenneth Hurwitz 25:20
it was very frustrating because I, my hand was shaky. And I couldn’t write on the whiteboard. One of the nurses put the whole alphabet on top of the board. And I was able to point but even that was hard, my hands was shaky. And I know they make devices, even children’s toys with the alphabet, which might be a good thing to do would be easier for people to point to a big block.
Just they wanted to try to do it on my phone with texting something, and then making it a voice. But I wasn’t able to do that. My hands were too shaky. And so it was very, very frustrating. And some of my dreams were like that, because when you’re restrained, and you have an 82. But in that was all my a lot of my dreams were just the frustration of trying to get people’s attention. And I’m trying to get them to come and see me. And you want people around you when when you’re when you’re in that condition. And I squeezed their hands which made me feel better. I mean, personal touch, human touch is a very needed thing.
Kali Dayton 26:30
You know, I noticed that when we were proning you and you were anxious, but you were so with it, I just we were trying all these ways to help you stay awake and cognitively intact, even while you were anxious and being prone. And it’s scary because you were needing higher ventilator settings, you were isolated. And yet you were so cognitively intact, or seemed to be, right? You were following directions you understood at that point, what was going on. And we felt like you were safe.
But we wanted to make sure you were comfortable. But we couldn’t be in the room all the time. But I noticed that, you know, as we’re trying to get your light sedation to the right level, if I rubbed your back, I could see the tension just relax. If someone gave you a hand, you would squeeze and hold on. I mean, even even in that kind of discomfort or even you didn’t feel like you’re totally cognitively there. It was just a human instinct to need human contact.
And that’s something so difficult about this COVID situations that we’re not always able to do that. And I worried with those first few days when you came. A lot of us were just poking her head out the window, trying to give you the thumbs up and say “hey, you’re okay”. But you didn’t have your cell phone with you.
So once you got your cell phone, I created a Google account that you could text the front desk and say what you wanted. So we have a couple of texts from you saying albuterol pump IV pump is alarming. Like you told us a couple of things that you needed. And then shortly after that, you need to be preowned, and you weren’t able to use your cell phone.
Dr. Kenneth Hurwitz 28:08
That was before I was prone, right. Yeah, that’s able to walk probably better. Because I was still in pretty good shape before I was prone, but after I was prone, I was pretty, pretty weak.
Kali Dayton 28:21
And that was eight days. After eight days, you became that weak. And you started out as an extremely robust, athletic man. You were in such good shape. I was amazed how you were doing push ups in the bed. At 30, I’m like, “I don’t know if I could be doing push ups after being intubated for six days”, but you really were you were that strong. But you’d be quickly became that weak, which was extremely impressive to me.
Dr. Kenneth Hurwitz 28:47
I lost over 20 pounds in this whole hospitalization game back about nine now. And I can do lots of push ups now and crunches and things like that. My recoveries gone pretty well. There was one or two days where my oxygen level would drop precipitously when I soon as I got up to go to the bathroom, I’d be like 94, 95 on oxygen while I have the cannula in two liters, sometimes three liters, then I’d get up and it would drop down to 82, 74.
And that happened for two days and we called our internist and I went to see her because I was worried that it was getting worse or I was getting it back again or I had some heart failure, Pulmonary Embolism, I didn’t know. He saw me and we did a an x ray and some blood work and my X ray actually looked a little bit better than the week before. So that was very reassuring.
And we just get through it that it was just a roller coaster of COVID getting better and then getting dipping down and getting better again and since that time Since that week, I’ve been steadily making progress. I can’t wait to go, I can’t wait to go to sleep. Because every day when I wake up, I’m a little bit better. And that’s that’s been the course I’ve been on. I still go off and still have a cough. Mostly when I’m talking. I don’t know if it’s from laryngeal spasm residual spasm, or from bronchospasm. I do use cell funeral maybe once or twice a day. Sometimes that helps. I’m not sure if it’s my vocal cords, or bronchospasm. I don’t really know I had a CAT scan today. At the hospital, I looked at it looked pretty good. But I’m not a radiologist. I really couldn’t say, what’s going on there. But I’ll find out the next day or so what kind of lung damage I had.
Kali Dayton 30:48
But you drove yourself.
Dr. Kenneth Hurwitz 30:49
I drove myself.
Kali Dayton 30:54
And on the podcast, we talk to other survivors of different treatments. And of course, the severity of illness has fluctuated so much. But some of these survivors that got sick in their 40s and 50s. Can’t drive now.
Dr. Kenneth Hurwitz 31:07
Really? Wow.
Kali Dayton 31:09
A lot of it’s because the cognitive impairments, they forget where they’re going. They don’t have the same response time. They’re just not safe to drive anymore.
Dr. Beverly Hurwitz 31:20
Beverly, she thought when I was coming home, I’d be a mess, right?
Well, I’d heard was that he was confused. And then when I speak to him, he was very focused on the bad dreams. And there was still some difficulty separating reality from these terrors that are haunting him. And I really was shaking in my shoes that the hospital was sending me somebody with neurocognitive neuro psychiatric impairments that I was really terrified that, you know, this wasn’t gonna be my husband anymore.
But it’s all, all that confusion cleared almost as soon as he got home, he spent the first night just telling me about the dreams. And then they just started to fade away. And he talked about them less the second night unless the third night and the became oriented to the life that comes with being at home. So yeah, I went from total terror of what his neurocognitive neuropsychiatric status was going to be to being astounded that, that the deficits were not there, I see a little bit of short term memory. Maybe that’s fine. But I can’t say I didn’t see a little bit before your COVID came into our lives. But I mean, he was home one day, and he was grilling me on what bills I had paid and knew the account numbers. And I was flabbergasted that his cognitive status was really good. Especially compared to what I was anticipating.
Dr. Kenneth Hurwitz 33:22
And I haven’t had any returns of those dreams. None at all. Been there in the past. I can remember a lot of them, I think maybe 14 or 15 of them. So I know some of them had to occur. While I was in the prone position probably or maybe four that I saw there was a whole number of them. And that could be cool most of them. But nothing really, really terrorizing just uncomfortable, uncomfortable.
Kali Dayton 33:49
So you don’t feel traumatized by them. You don’t have PTSD?
Dr. Kenneth Hurwitz 33:55
They’re just an experience I had as well.
Kali Dayton 33:58
We were so excited for you to go home in part because we knew it would help expedite your recovery. I just wanted…. I just had the suspicion that once you were home that that alone would help your delirium and your cognitive function.
Dr. Kenneth Hurwitz 34:12
Yeah, it did. When I came home I milked it a little bit with Beverly I made her do a few things that I could have done. But she snapped the whip and I’m doing a lot every almost everything by myself.
Dr. Beverly Hurwitz 34:28
He could do 25 pushups and 50 crunches but he still couldn’t open the dishwasher door. haha
Kali Dayton 34:36
Amazing how that happens, right? haha And Beverly when I’m when I was talking to you one night. I think this is right before he had to be proned. I explained that he was anxious but yet, CAM negative didn’t seem to be delirious, but he doesn’t seem to be fully himself and explained why we were avoiding sedation. You said, “Thank you so much for having a neuroprotective protocol.” As a neurologist, what did you mean by that?
Dr. Beverly Hurwitz 35:11
Well, I’ve always told my patients that for every day you spend in bed it will take a week to recover from the physical and, and psychological gold burden of of losing that time for activity and function. And maybe when I say neuroprotective, I was thinking neurocognitive neuropsychiatric, but also neuromuscular because the body is a machine.
If you stop moving, the rest sits in. If you take a long car ride, your knees might stiffen. When you get up in the morning, you might have to stretch because the Russ was setting in even the eight hours that you weren’t weight bearing on your spine. So I’ve coming from a neuromuscular clinic background mobility is extremely important to all function. And then it can on top of that it at the neurocognitive and neuropsychiatric facilitation caused by being intubated, unconscious, sedated on neuro nasty drugs.
Yeah, I when you told me that. I mean, when I was told he was intubated, I haven’t done hospital medicine. I’ve been an ambulatory medicine, since I finished Fellowship, which is almost 40 years ago. But I, you know, my thought was, “well, he’s going to be unconscious and paralyzed.” That was the only way I knew.
And I was just just so ecstatic to hear that he was awake, that he was receiving physical therapy intervention on those first few days. And I was just applauding that your ICU wasn’t keeping him in a coma and paralyzed I was astounded that that happened. And I talked to other colleagues who are related to critical care or got drafted into critical care when COVID did. And they were all astounded at what was being done in the ICU. Ken was in relative to what they were doing in Miami, and Dallas, Hartford, Connecticut, where we have friends and relatives who, who were either practicing critical care or got drafted into.
Kali Dayton 37:51
And now that he’s home, your five weeks, six weeks later, six weeks. So Beverly, what does it mean to you now, in the context of normal life, not just that he survived, but that he’s home with you and functioning? What does that mean to you and your life?
Dr. Beverly Hurwitz 38:10
Well, I’m I went through a period of a week where I had no idea if he was going to survive, and then a week where I didn’t think he was going to survive. Right up to the day that I was asked if I wanted to do not resuscitate order over his bed. And I was anticipate he got worse from that point for another few days. And I was anticipating the pull the plug question.
So I went from psychiatric depth of despair. You know, I had this extremely healthy, robust spouse of almost 50 years, and I’m going to say goodbye, and then an alternative. So, yeah, I feel like I’ve been on quite the seesaw ride. And it’s just so amazing that not only did he survive, and not only did he walk into the house, because I fully expected him to go to a rehab hospital. But that yesterday, he was out on the golf course playing golf.
Dr. Kenneth Hurwitz 39:23
I was in a cart there. So it’s kind of cheating.
Dr. Beverly Hurwitz 39:25
Yeah, we’re normally walkers. We normally walk he calls we walk to the course we welcome the course. So yeah, I’m just like, over the moon, that not only did he turn around, but he’s achieved a level of rehabilitation that I could not have anticipated.
Dr. Kenneth Hurwitz 39:47
I tell everybody that. For me. The journey wasn’t terrible, but for Beverly and the people who love me. They’re the ones who really suffered and they’re the ones who had the burden No, my illness I didn’t know what was going on. And in fact, during my, when I had my birthday Monday, I told people that this is my second birthday, or my rebirth day, because not many people get the chance to come back and live again. And I’m so grateful, and I can’t thank you guys enough. I’m just so grateful for the care I received there.
Dr. Beverly Hurwitz 40:26
I do have a thought to add to your evaluation of how these COVID patients progress through this whole experience of ICU delirium. In that he can’t remember much of anything from the initial period of our viral infection. He doesn’t remember the day that I was running in circles trying to get a home oxygen unit, he doesn’t remember he was coughing so violently that that the house was shaking.
And I can remember almost every day of those 12 days of us having all these nasty illness symptoms. And so I really think COVID attacked his brain, that all of that is is unclear. And his recall as is most of the ICU experience is not remembering even before he wound up with hypoxic and in an ICU. But I can tell you that that whole 10 days was terrible insomnia. Anorexia, for him, non-stop coughing, fever, chills, body aches, some nasty flu like illness, but it had far more effect on the brain than any
Dr. Kenneth Hurwitz 41:56
Well, I thought it would end at 13 days. It was hoping for the 13th day most people had it for two weeks. I said, Okay, two weeks is up. And I should be better by now. But I wasn’t. Yes, if that was from somebody, I don’t know who was.
Kali Dayton 42:13
well, you hit, you hit that cytokine storm, and you you got it hard. And I think that’s an important point for the critical care world, as with influenza, with a lot of the septic kind of patients that come in pretty promptly after getting sick. And a few days to a week, you had already gone through 13 days of poor nutrition, decreased in activity, neurotoxicity.
And so it is even more important not to exacerbate all of that- to implement these things that we know to try to keep them active and awake and protect their body and brain that are already so deconditioned from this prolonged illness that they’ve suffered at home. That’s been happening for before us. And I think some of the there’s so much fear with COVID.
And very, very reasonably so you were so sick, and that you were that patient that everyone’s calling in on their off shifts asking if the only question was How is room 45? But it was more. But the real question is, is he still alive? That’s what everyone really cared about and wanting to know. Is he still with us? Is there still a chance because we were working so hard to keep you live? And so these outcomes were not because you didn’t get sick? Because you weren’t critically ill. And so the fear is, you know, people say but my patients are really sick, so we have to sedate them the second they’re intubated. But they really make such a good point.
That these are people that are so sick, it’s even more important to protect their brains and bodies while we can, so everyone’s course is different, but because kan came to a unit that kept them awake and walking for six days. Still awake for another two days while preowned and then sedated for six days because absolute necessity. He was able to wake up again, get back on his feet. And five, six weeks later be shooting a round of golf at 70 years old.
Dr. Kenneth Hurwitz 44:18
Exactly. So I can’t say how grateful I am. As many times I’m just astounded that people helped me like that. So grateful.
Kali Dayton 44:30
Well, you and all our patients are worth the fight and I’m so glad you’re getting your life back. And I’m sure you’ll be right back to walking your full…
Dr. Kenneth Hurwitz 44:39
18 holes
Kali Dayton 44:40
18 holes, I can’t even talk golf!
Dr. Kenneth Hurwitz 44:42
at the end of the summer. Maybe sooner. I don’t know
Kali Dayton 44:47
You have a good wife to take care of you and neurologist on hand all the time.
Dr. Kenneth Hurwitz 44:53
I have the best wife in the world…. she’s so great.
Dr. Beverly Hurwitz 44:57
I will say that He oxygenates better when he’s mobile. And when the therapist first came, it was kind of like he was an orthopedic patient, let’s get your strength. And he was very good condition. So that was important. And it was like he was a stroke patient, let’s work on your coordination and balance, but it wasn’t aerobic.
And he do this hour of strength balance. And then he’d be exhausted. And I’d say, he wants something a glass did you say, get up? Whoa, atelectasis Electus isn’t gonna get better if you’re not moving. And it took a while not only of me being a nag at him, but to start nagging a therapist to push him to do aerobic. And once he started to do more aerobic and be more mobile, that’s when his COVID curve stopped undulating and started to really for to go progressively. So mobilization not only was critical to his survival, but I think it’s been critical to his recovery.
Kali Dayton 46:16
Right, and we find ARDS patients have a high rate of readmission to the ICU. Usually, because they’re so deconditioned that they leave the ICU and then they don’t keep working on their mobility, though, they don’t get stronger than they can’t clear the secretions. They have repeated pneumonia or different, you know, they still have Foley catheters or different things, because they’re still hospitalized. They have a really high re admission rate. Yeah, I do not see Ken having to come back to us anytime soon.
Dr. Kenneth Hurwitz 46:48
I’m not going back, I don’t want to to see you again, in the hospital.
Kali Dayton 46:53
It’s okay, I’ll see you at the grocery store, but not at our unit. But you’re doing your part. And we’re so excited and so proud of you. And it’s just a wonderful validation to the unique and bizarre approach that we take to critically ill patients that I hope will be standard. And thanks for sharing your experiences that help us understand the bigger, bigger picture of why we do what we do.
Dr. Kenneth Hurwitz 47:18
Please give everybody my best. And tell them how well I’m doing. I appreciate that.
Kali Dayton 47:24
I will and you know what? I’m going to have a listen to this so they can hear from you. You told me I can. Thanks so much, guys. Thank
UPDATES: 2 weeks after this interview, Dr. Hurwitz emailed me with the report that he walked 8 miles golfing only 8 weeks after discharge from the ICU. He has resumed his passions such as skiing and exercising. He is enjoying full quality of life.





Transcribed by https://otter.ai
SUBSCRIBE TO THE PODCAST




