Despite many exciting advancements in technology and research, ICU sedation and mobility practices continue to be stuck in the past.
A big part of this problem stems from ICU culture, which encourages clinicians to fear change and be resistant to new ideas and approaches.
But regardless of these issues with ICU culture, the truth is, the majority of clinicians want nothing more than to save and preserve as many lives as they possibly can, and they’re willing to do what it takes to make that happen.
Unfortunately, as I’ve learned after several years of attempting to improve this regressive ICU culture, changing the minds of those who work in the ICU can be incredibly difficult, no matter how much supporting evidence you can provide.
Luckily, the push to align sedation and mobility protocols in the ICU with current research is gaining ground, and one of the reasons for that is the use of simulation training.
Simulation training has been used for many new skills and protocols in medicine for decades, but when it comes to teaching ICU clinicians about sedation and mobility practices, it is an underutilized approach.
So, I figured I should publish an article on simulation training, explaining what it is, how it works, how it can benefit your ICU, and why our approach can help to inspire much-needed change.
What Is Simulation Training?
Simulation training is a type of exercise where individuals are exposed to realistic scenarios or situations that mimic real-world experiences in a controlled environment.
The purpose of simulation training is to provide a safe environment for individuals to practice and refine their skills without the risks associated with real-life situations.
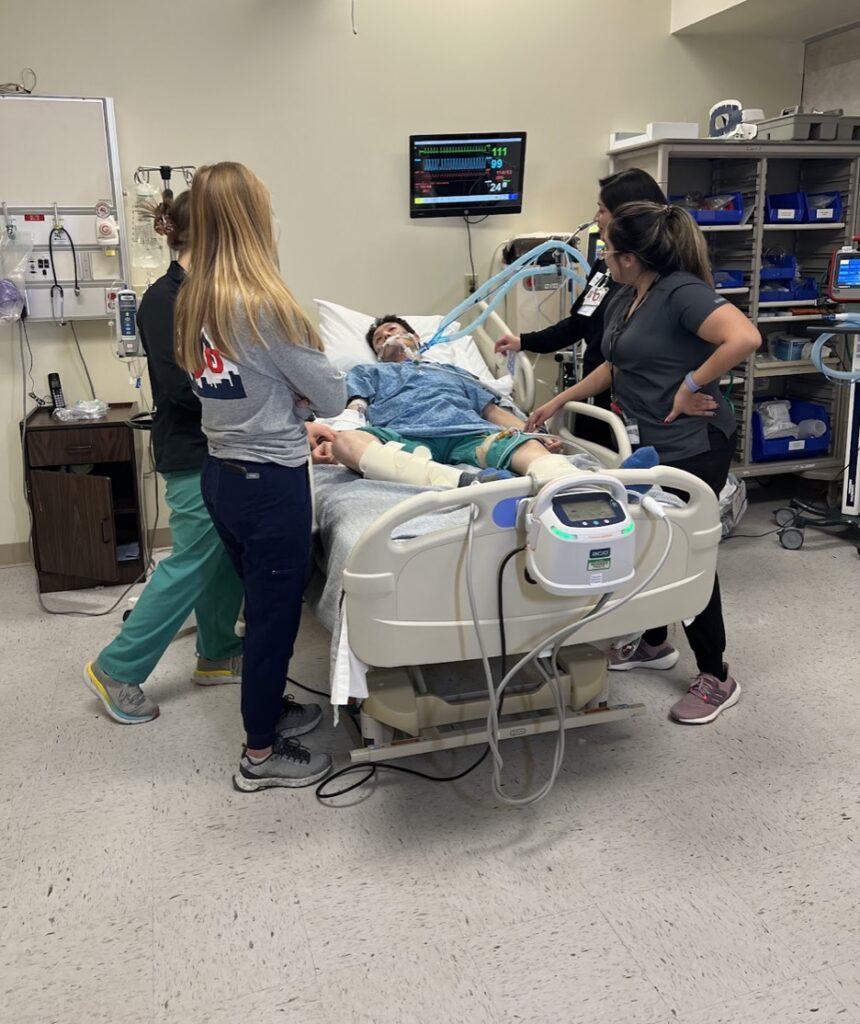
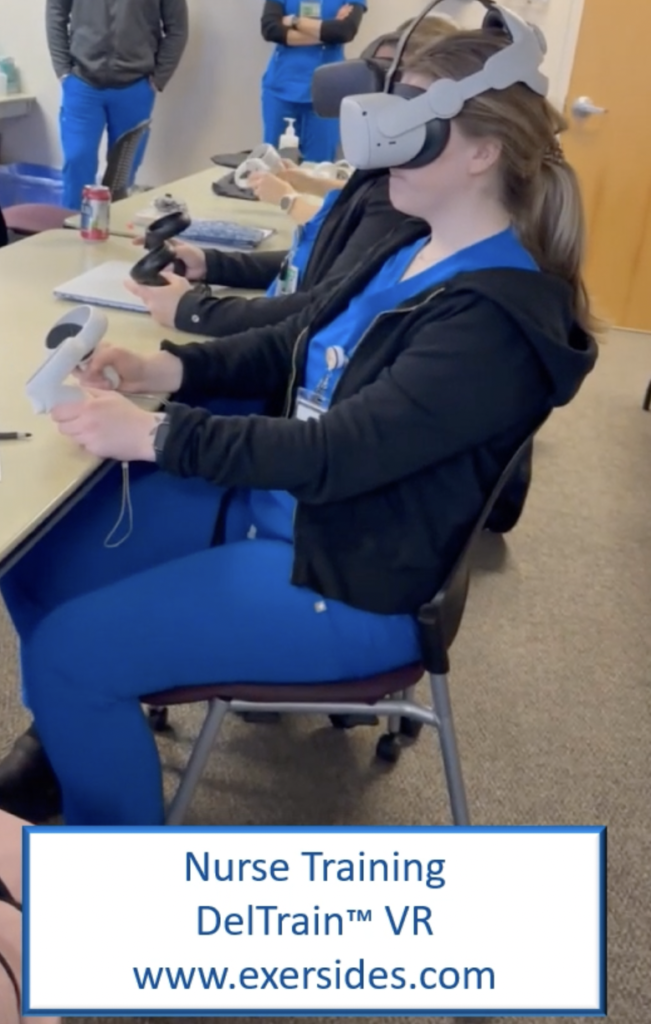
In the context of the intensive care unit, simulation training involves the use of role-playing exercises, mock scenarios, computerized mannequins or real actors, virtual reality technology, and other advanced equipment to create a simulated environment that replicates real-life ICU scenarios.
Clinicians are presented with various case studies, and they must work together to manage each simulated patient’s care. The simulation environment can also be customized to replicate different levels of acuity, from stable patients to those in critical condition.
During the simulation, clinicians are closely monitored by trainers who provide feedback on their performance and offer guidance on how to improve their skills. The simulation can also be paused at any time to offer feedback or allow the team to discuss their approach to managing the patient’s care.
This type of training is designed to prepare ICU clinicians to handle various critical care situations and to improve their clinical skills by allowing them to practice in a safe and controlled environment, without the risk of harm to actual patients.
How Does Our ICU Simulation Training Work?

When we work with ICU teams, we utilize real people acting as patients to facilitate behaviors and responses that realistically mimic ICU patients experiencing various levels of sedation, delirium, and weakness.
Typically, these actors will be lying in a hospital bed with a gown on, with lines and tubes connected to them to make it look like they’re intubated, for instance. Ideally, we’ll also have the monitors going, making sure everything is as realistic as can be.
Before we begin, we assess for baseline knowledge by evaluating clinicians’ participation in our webinar sessions. We do this because our simulation training is most successful when attendees have foundational knowledge about delirium, ICU-acquired weakness, and early mobility, and understand the importance of being part of an Awake and Walking ICU.
We then initiate the training by leading a discussion with the attending clinicians to ensure they understand that simulation training is a judgment-free space for learning, experimenting, and collaboration.
We’ll then describe a scenario, such as an 85-year-old woman named Betty with a history of diabetes and hypertension who has been admitted to the ICU for urosepsis, and explain that upon arrival, she was intubated and continuous Propofol was started at 30 mcg/kg/min and fentanyl at 75 mcg/hr.
At this point, we’ll start asking clinicians questions, like:
- What are your concerns about this scenario?
- Does Betty have an indication for sedation?
- What are her risk factors for delirium?
- What are her risk factors for ICU-acquired weakness?
- How would delirium and ICU-acquired weakness impact Betty’s life?
Then, once we’ve gone over all these questions, we’ll ask something like, “Okay, understanding all of this, what’s your next step? And what’s your top priority?”
In this case study, the top priority might be for Betty to get off of sedation and mobilize as soon as possible. After explaining that to the clinicians, we’ll work with them through each and every step of the process, stopping at any time for questions or clarifications, and even having the actor change their presentation based on how the scenario is playing out, if need be.
The idea is to make sure that clinicians fully understand how the evidence-based practices being described will affect the patient’s outcome, and what they’ll need to do to adhere to these protocols if and when this scenario actually happens.
What Are the Benefits of ICU Simulation Training?
The use of ICU simulation training offers many benefits for all stakeholders, including patients, clinicians, and the hospitals where they work. This includes things like:
- Improving patient outcomes
- Enhancing communication skills
- Ensuring greater collaboration between ICU team members
- Giving clinicians the ability to ask questions and address concerns
- Improving the competence, confidence, and decision-making abilities of clinicians
- Allowing clinicians to gain experience managing complex and challenging patient cases
- Helping to shift ICU culture away from the use of outdated and often harmful practices
- Providing a safe and ethical way of exposing clinicians to certain procedures or situations
- Identifying potential errors before they happen, which allows clinicians to practice strategies to prevent these kinds of things from happening in a real-life scenario
Sadly, in spite of all these benefits, simulation training is rarely used to train teams on sedation, delirium, and mobility management. But that doesn’t mean there isn’t plenty of evidence to show that it’s a well-founded and effective form of education.
For example, according to a review published in Medicine, “Simulation-mediated education offers learners a safe practice environment where they can engage in critical thinking without endangering themselves or others who might otherwise be subject to harm in a real-life event.”
In addition, a Journal of Education and Health Promotion review concludes that “In teaching health information systems…simulation training improves the skill, attitude, knowledge, and satisfaction of students and health-care providers including physicians and nurses,” and an article from StatPearls states that “It is a chance to work on team skills and improve learning in a controlled environment while still maintaining the challenges presented by context, distractions, and practical difficulties.”
What Makes Our Approach to Simulation Training so Much Better?

Unfortunately, oftentimes, simulation training isn’t nearly as effective as it could be.
There are many different reasons for this, and here at Dayton ICU Consulting, we’ve done our best to address each and every one of these shortcomings.
Below, I’ve outlined a couple of unique aspects of the way we do simulation training, and explained why these methods make our approach so much better.
Greater Collaboration
In many ICUs, when simulation training is offered, it’s all too common for only a couple of “champion” clinicians to participate. They are then expected to teach the rest of their team at the bedside during regular patient care interactions.
This method tends to be ineffective, as clinicians are still not experts after brief training, and are busy with their regular patient load. It is an impossible requirement for these “champions” to be charged with the task of converting, educating, and training their colleagues.
With that in mind, when we work with ICU teams, we try to ensure that every single member can attend simulation training on day and night shifts.
We invite all disciplines to attend so that pharmacists, physicians, advanced practice providers, physical therapists, occupational therapists, respiratory therapists, and nurses can practice communication, collaboration, and critical thinking together through sedation, delirium, and mobility management.
In addition, we strongly encourage participants to watch our series of webinars before we even arrive on-site, so everyone’s on the same page before the training even begins.
Real Case Studies
Unlike many other forms of simulation training, we primarily use real case studies.
Instead of creating a fictional scenario, most of our case studies are based on patients that we have treated or survivors that have shared their journeys with us, and many of these case studies have been documented on our website, and/or discussed on my podcast.
What’s more, clinicians who participate in the training can access these additional resources via a QR code on the handouts we give them, so they can get further context after the training by reading and/or listening to these patients’ stories.
These real case studies and survivor testimonials help to ensure that our training is patient-centered, and this is incredibly important, because it acts as a continual reminder of the impact our practices have on the trajectory of patients’ lives.
The Effect Our Training Can Have on Clinicians
I have observed that clinicians often enter the training with trepidation and hesitation to perform new skills with a new approach.
But by the end of our simulation training, the shift in their enthusiasm, perspective, and confidence is palpable. They leave with excitement to utilize these new tools in their practice, and they feel supported and united by the collaboration with their colleagues.
Moreover, after attending our simulation training, many clinicians report increased success and greater momentum in applying evidence-based practices and becoming Awake and Walking ICUs.
Do you want your ICU team to participate in evidence-based simulation training? We can walk you through the entire process, so please don’t hesitate to contact us.




