Despite all the evidence to the contrary, most ICUs still operate as if the best thing you can do for patients on the ventilator is to ensure they remain sedated and immobile.
But the truth is, there are mountains of evidence to show the harm that these practices can cause for ICU patients, and just as many studies that show the benefits of doing the exact opposite.
Slowly but surely, ICU clinicians around the world are beginning to admit that their previous approach was wrong and starting the process of implementing evidence-based sedation and mobility practices.
Unfortunately, most ventilated patients don’t get to experience this kind of care, but when you analyze the outcomes for the lucky few that do, the benefits couldn’t be more obvious.
I love highlighting these kinds of positive outcomes for patients who do receive the kind of evidence-based care outlined in the ABCDEF Bundle, and the case we’re about to look at offers a great example.
It involves a woman who could very well have died or had her quality of life destroyed had she received conventional care, but she was lucky enough to be admitted to an Awake and Walking ICU.
Her name is Joan, and this is her story.
How the ABCDEF Bundle Preserved Joan’s Quality of Life
Joan is a 38-year-old woman with a history of tobacco use who was admitted to an outside hospital in September of 2018 for acute respiratory failure secondary to influenza, which then devolved into acute respiratory distress syndrome (ARDS).
She required mechanical ventilation, but fortunately for her, she was transported to the Awake and Walking ICU, which adheres to the evidence-based practices found in the ABCDEF Bundle.
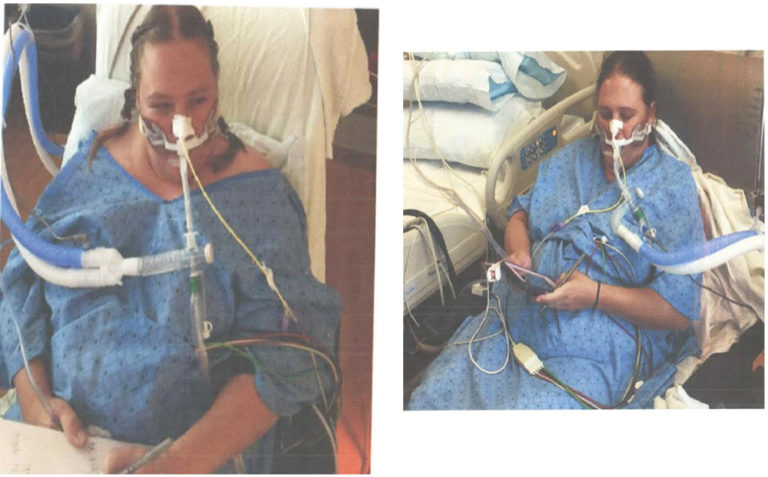
Joan was immediately liberated from sedation and allowed to wake up and mobilize for the rest of her time on the ventilator.
Her mild ARDS persisted, and for many days, her ventilator settings were sitting at a PEEP of 12 and an FIO2 of 60%.
In spite of her illness, Joan was able to text staff and family on her phone, walk, help her kids with their homework, and play an active role in her recovery.
She had an unprecedented gag reflex that is not present in most patients, but still, she stayed calm and tolerant of the tube because she was free of delirium.
“It was horrible. I gagged constantly,” she said when I asked her about what it was like being awake on the ventilator.
When asked how she dealt with this discomfort, she said, “I think it was just the will to survive. I had realized that, you know, I’m not getting out of here unless I do something about it.”
Joan also reports having terrible experiences while under sedation during her transportation to the Awake and Walking ICU and said she would have preferred to endure gagging on the tube rather than having to deal with the terrors she suffered while she was sedated.
Luckily for Joan, she only spent about 12 hours under sedation, as she was airlifted to a different hospital, but she still had to deal with some incredibly disturbing hallucinations, including feeling like one of the nurses was trying to cut off her hand.
“He was just sawing into my wrist. And he kept telling me I’m so sorry. I’m so sorry. And I could have sworn he was sawing my wrist off,” she said.
When I asked her why she preferred to remain awake, rather than be sedated, she said, “If I had to go through that for 17 days, I think I would have been…you would have to put me in a loony bin.”
By the time she was ready to leave the ICU, she was able to walk more than 1000 feet at a time, despite being on the ventilator.
“My nurses and everybody just kept pushing me and said if you want to get better…you’ve got to get up and walk. So, to be able to get up…it’s huge,” she said.
Believe it or not, because she was awake and mobile, Joan was even able to take showers while on the ventilator, which provided her with some much-needed comfort and dignity.

As you can see from the image above, in order to facilitate this, the nurses who treated Joan had to wheel her ventilator right down to the shower.
“The very first time was very unpleasant,” she said, explaining that at the time, she wasn’t even able to wash herself without help from the nurses.
But with a lot of determination, and the dedication of the ICU staff, Joan was eventually able to take a shower all by herself. “That was probably my favorite part,” she said.
Then, after 17 days of being intubated on mechanical ventilation, Joan was successfully extubated.
And as a result of the evidence-based care she received in the Awake and Walking ICU, she was able to walk out of the ICU doors and go straight home from the hospital.
What’s more, only a few months after her discharge, she was back to running her own business.
“I’ve heard other ARDS patients where they say, ‘I’m losing my house and everything,’” she said. “I was so blessed to come back to work soon.”
Joan later joined an ARDS survivor support group on Facebook.
Thankfully, she was unable to relate to most of the conversations this group was having, as she does not suffer from things like post-ICU PTSD, cognitive deficits, tracheal stenosis, or the long-term effects of ICU-acquired weakness.
“You know, most of the ARDS patients I can’t relate to because I wasn’t sedated. I was awake through the whole entire thing,” she said.
“Being awake is so rewarding. I would not change it for anything, as much as the pain. It was the worst pain I’d ever went through. It was the worst nightmare I’d ever went through. But I wouldn’t change it. I’d still want to be awake again.”
At any rate, the choice to allow Joan to wake up and mobilize while she was on the ventilator was likely responsible for saving her life, not to mention sparing her the costly repercussions of sedation and immobility.
In the end, it allowed her to preserve her quality of life and continue to provide for her family in the face of what could have been a grave illness.
If you want to learn more about Joan’s story, from the woman herself, you can hear her talk about her experiences in the Awake and Walking ICU on Episode 17 of my Walking Home From The ICU podcast.
Are you ready to do what’s best for your patients, your ICU team, and your bottom line, by implementing the most up-to-date, evidence-based practices? We can walk you through the entire process, so please don’t hesitate to contact us.



 When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team.
When patients are so ill that they require a ventilator in the ICU, the antiquated approach of heavy sedation and immobilization should be avoided in order to help prevent the immense burden of physical and cognitive disabilities suffered during survival. To understand this better, listen to Walking Home From The ICU. You will see what ICU consultant Kali Dayton provides to your team.
