Most patients who are admitted to the ICU in need of mechanical ventilation have to suffer through days or even weeks of deep sedation, immobility, and all the ill effects of these practices.
But for patients with acute respiratory distress syndrome (ARDS), this lack of adherence to evidence-based practices can spell the death of their quality of life, as many of them end up dealing with horrendous side effects after they leave the ICU.
This includes everything from hospital readmissions and cognitive impairments, to myopathy, and even post-ICU PTSD and dementia.
And in addition to all of this suffering, after being discharged from the hospital, a lot of ARDS survivors are unable to return to work, and even if they do, many of them are only able to work reduced hours.
But every once in a while, an ARDS patient is lucky enough to receive evidence-based care, and in these instances, the outcomes of their care are radically different, and much more positive.
This is made possible because these ICUs adhere to evidence-based practices, like maximizing mobility and minimizing sedation.
That being said, these examples show just how different things can be for ARDS patients if the ICU teams that treat them do what’s in their best interests.
So, to cap off my case studies for the year, I figured I should highlight another one of these examples, and really drive home how important it is for ICUs to be following these evidence-based practices.
This case study involves a man who was severely ill with ARDS, but as a result of the evidence-based care he received, his quality of life, which could have been destroyed, was pretty much perfectly preserved.
His name is Tyler, and this is his story.
How Evidence-Based Practices Saved Tyler’s Quality of Life
Tyler Lintz was a 32-year-old firefighter when he was admitted to the ICU for septic shock secondary to group A streptococcus pneumonia.
He was intubated in an outside facility and then transferred to the Awake and Walking ICU.
Upon arrival at the Awake and Walking ICU, he was liberated from sedation and continued to require vasopressor support for his septic shock.
He recalls experiencing intensely vivid hallucinations while he was sedated.
Tyler, being a firefighter, explained that in one of these “dreams” he was on a search and rescue team during a big storm in New York, but then got into a severe accident in the fire engine and ended up breaking his neck.
The next thing Tyler knew, he was waking up strapped to a hospital bed with tubes sticking out of his body, and he could have sworn he was in the hospital being treated for that broken neck.
Waking up like this without any context was quite scary for Tyler, who said he was in a state of “complete confusion” at the time and was “very anxious.” He also made a point of saying that even while he was sedated, he could still feel the anxiety.
In any case, despite being delirious from the sepsis, he was promptly ambulated and was able to walk about 75 feet.
The videos below show Tyler being ambulated, and they really do justice to what an accomplishment this is for someone who just woke up from sedation.
As someone who was very physically fit before being admitted to the hospital, Tyler remembers how difficult it was to end up losing 35 pounds and struggle to sit up in bed or even squeeze a stress ball.
“It was very depressing. I literally had to learn to walk again. I couldn’t remember how to walk. You know, there was, ‘Put your right foot out, put your left foot out, your gait is too linear, spread, spread your hips,’ and it’s just so frustrating, you know?
“I started thinking, Holy crap, I’m going to stroke out – just with the ECMO and everything else. Are they pushing me too hard? You know because I’ll keep going. But should I not keep going? It’s just a mind game,” he said.
The next day he started to develop acute respiratory distress syndrome (ARDS), but he continued to be mobilized.
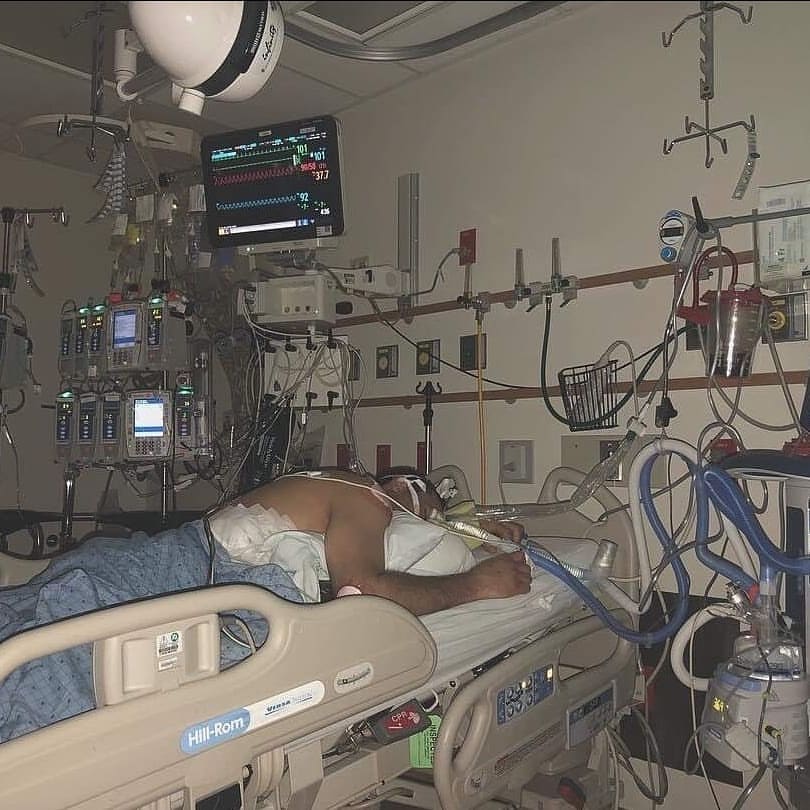
As you can see in the image below, after about 48 hours, he was unable to oxygenate with movement and required pronation, deep sedation, and paralysis.
At this point, the decision was made to transfer him to a neighboring hospital for what’s known as extracorporeal membrane oxygenation (ECMO).
During this procedure, blood gets pumped out of your body and into a machine that removes carbon dioxide before sending the oxygen-filled blood back to the tissues in your body.
The point of this procedure is to allow blood to circumvent the heart and lungs, giving them a chance to rest and heal, and it’s commonly used for ARDS patients who are unlikely to survive using conventional therapies alone.
Fortunately for Tyler, his new cardiovascular intensive care unit (CVICU) also had a strong culture of prompt ambulation for both ECMO and mechanical ventilation.
As someone who experienced being in the ICU with sedation and without, Tyler said he would much rather be awake, and described being sedated as “very anxiety-ridden depression.”
“There were times where I would come off the sedation, and then whatever we were doing the bike or trying to sit up or just something, and then all of a sudden, they’d be like, I remember, ‘We’ve got to sedate him again’ and I’d just go back into delirium mode, hallucinations. I remember being awake, semi-consciously, but I would see things in my room. You know, it wasn’t comforting.”
Tyler’s wife Amber was also very grateful that he was given the chance to remain awake in the ICU.
“I much preferred him awake,” she said. “Because he was showing me that he was making steps to get out of there. And I needed those small little things to show me that he was progressing. Even like, you know, squeezing my hand, or opening his eyes, things that small were huge to me, because it was just like, okay, he’s doing something.”
Then, shortly after being placed on ECMO, sedation weaning began.
All told, Tyler spent about three weeks on ECMO and walked on ECMO for about two weeks before the procedure was discontinued.
After this, he spent an additional three weeks in rehabilitation and was then able to discharge home.
If you want to learn more about Tyler’s story, from him and his wife, Amber, you can check out Episode 18 and Episode 19 of my Walking Home From The ICU podcast.
How Tyler’s Doing Now Versus How Things Tend to Go for ARDS Survivors

It’s incredible that Tyler was able to recover as well as he did, especially considering how tough things can be for people with ARDS, even when they do survive.
In spite of all of this, about two months after his discharge, Tyler was able to start working as a firefighter once again, and a few months after that, he was promoted to chief of his department.
But typically, ARDS survivors face significant challenges and changes after their hospitalizations, and the stats below will give you an idea of just how bad things can get, and how lucky Tyler was to have been admitted to ICUs that actually adhere to evidence-based practices.
- 83% of ARDS survivors are readmitted within the first two years after discharge.
- 25% of them are readmitted within the first 30 days after discharge.
- 70-100% of ARDS survivors have cognitive impairments upon discharge from the hospital.
- 46-80% of ARDS survivors still have cognitive impairments (post-ICU dementia) one year after discharge.
- 48-96% of survivors still have myopathy (muscle weakness, cramps, stiffness, or spasms) two years after discharge.
- Only 68% of ICU survivors ever return to work.
- Of that 68%, 43% end up working reduced hours, 27% report having reduced capacity, and 24% will eventually lose their jobs.
In any case, much of the damage and deficits faced by ARDS survivors can be attributed, at least in part, to a lack of adherence to evidence-based practices, which leads to prolonged sedation, delirium, and immobility during mechanical ventilation.
On the other hand, the approach taken by the Awake and Walking ICU teams that cared for Tyler, which involves following evidence-based practices by minimizing sedation and maximizing mobility, has allowed him to return to his family, career, and life without any serious side effects.
He is free of post-ICU PTSD and post-ICU dementia and is currently leading a fulfilling life with a successful career.
The Awake and Walking ICUs that preserved his function by avoiding sedation and immobility during his critical illness truly saved not only his life as a whole, but also his quality of life.
Are you looking to implement evidence-based practices in your ICU? We can walk you through the entire process, so please don’t hesitate to contact us.




