While it’s clear that the ABCDEF Bundle saves lives and helps to restore the quality of life for ICU survivors, many intensive care units continue to standardize deep sedation and immobility.
But why is this?
Why does one ICU use sedation on less than 20% of intubated patients, while another sedates 100% of these patients into medically-induced comas?
And why do patients suddenly start mobilizing when they’re transferred to an ICU that prioritizes early mobility, even when their medical status has not changed?
With these questions in mind, it’s important to understand that ICU culture is one of the main barriers to creating Awake and Walking ICUs, which prioritize evidence-based practices like early mobility.
The Merriam-Webster dictionary defines culture as “a set of shared attitudes, values, goals, and practices that characterize an organization and shape the behavior of its members.”
Unfortunately, the outdated attitudes, values, goals, and practices of much of the ICU community are often exposed throughout the internet.
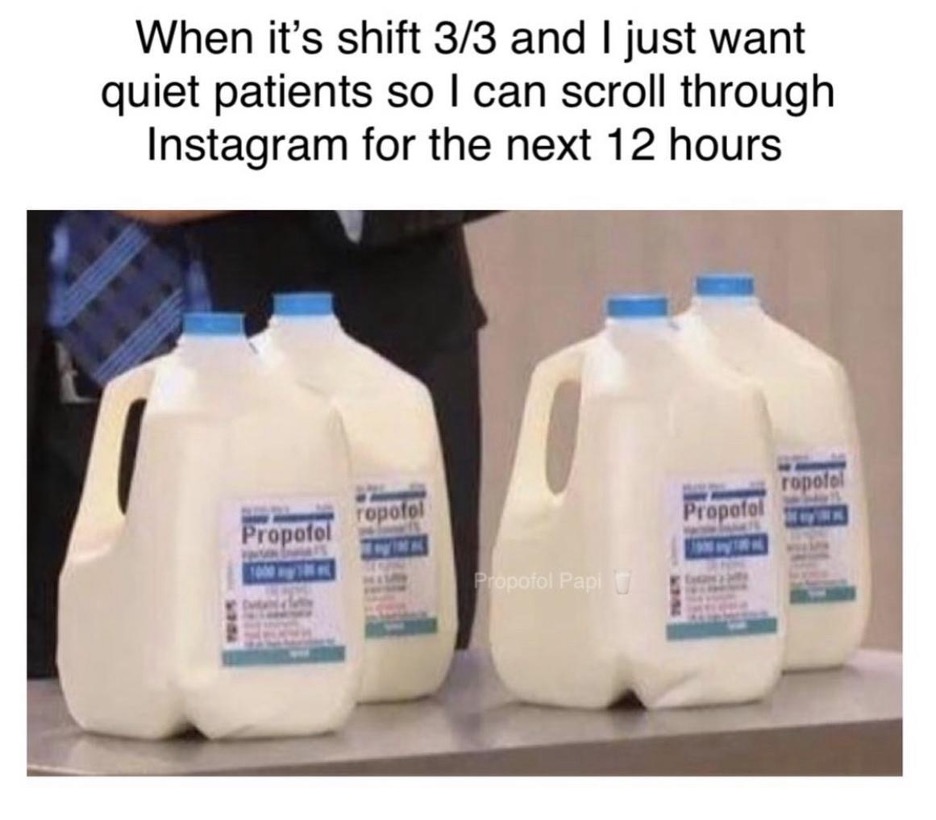
Decades of prevailing ICU culture, which prefers to keep ventilated patients comatose and immobile, is expressed, particularly through memes on social media, many of which have been shared tens of thousands of times.
Over 10 years ago, as a younger travel nurse, I too chuckled at jokes like these:
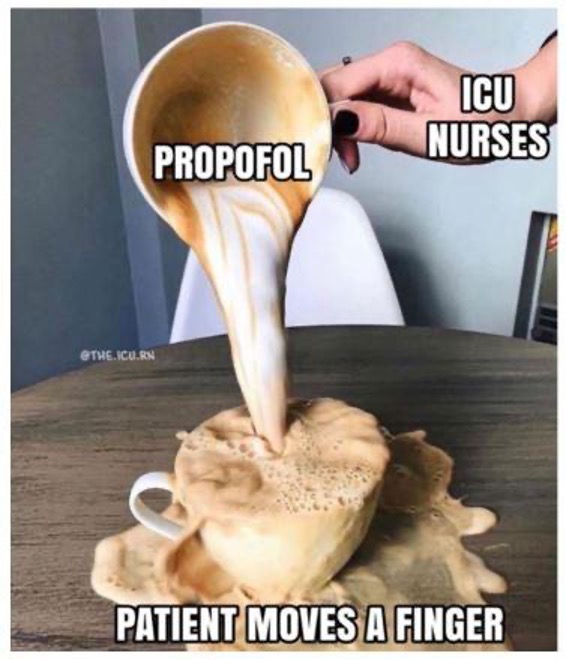
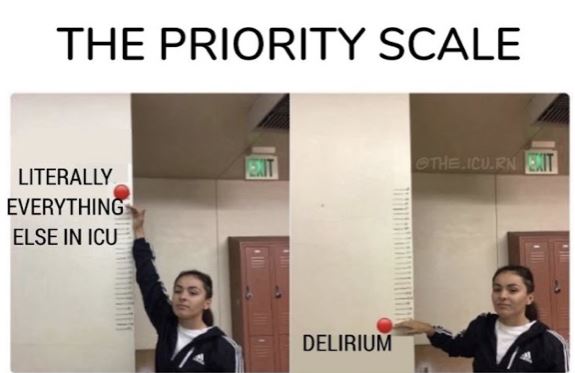
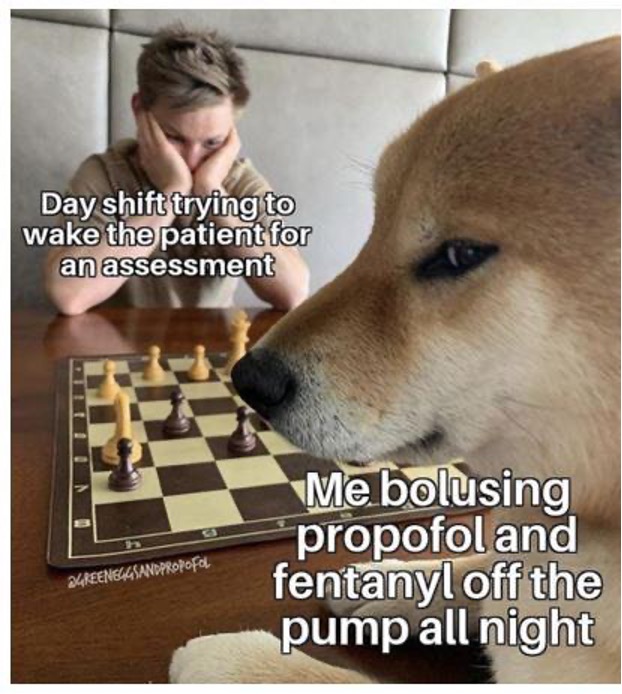
But what I didn’t know was that I was laughing at increasing patient death, suffering, and disability.
Unfortunately, it is memes like these that truly reveal the influence ICU culture has on bedside practices.
For instance, when I asked my Instagram followers if these “jokes” existed at the bedside in their ICUs, 94% of respondents said yes.
And when I asked if they believe that this influences practices at the bedside, 97% said yes.
All things considered, there’s no denying that ICU culture is a significant determinant of whether patients will be sedated and immobile or awake and ambulating.
However, the prevailing ICU culture of automatic and persistent sedation and immobility exists not because clinicians don’t want to provide the best care and outcomes for their patients, but because they don’t understand how these interventions affect patients during and after the ICU.
Knowledge Gaps in ICU Culture
One of the main reasons why ICU clinicians fail to create Awake and Walking ICUs is that they lack the knowledge required to understand the why and how of the ABCDEF Bundle.
With that in mind, here are some of the knowledge gaps in the ICU that are preventing the implementation of these evidence-based practices:
Sedation
Numerous gaps in education have molded ICU culture and, in turn, the beliefs and practices that it promotes.
One of the biggest gaps for ICU clinicians is their lack of understanding of the risks of sedation.
ICU clinicians are not taught the risks of sedation and instead are led to believe that patients are peacefully sleeping while they’re sedated.
For instance, a survey published in the American Journal of Critical Care found that 66% of ICU nurses believe sedatives are necessary for patient comfort.
Moreover, surveys have found that 59-77% of ICU clinicians would want to be sedated if they were intubated.
As you can tell, when clinicians are not exposed to the survivor perspective and fail to understand the increased risk of death, brain injury, trauma, and disability that comes with prolonged sedation, the myths that sedation is “sleep” and “humane” continue.
This misunderstanding acts as a justification and can increase clinicians’ personal preference for sedation and influence how they sedate their patients.
And because sedation is seen as benign, jokes are often made about it, both on and off the unit.
Sadly, most ICU clinicians are unaware that what they’re actually joking about is the increased suffering and death that their patients have to endure.
When nurses resume sedation, patients return to being motionless and they feel they have “fixed the problem” by “returning patients to their slumber.”
But until clinicians understand the torture patients endure while sedated, they will continue to think this “humane approach” is something to be laughed at in memes and perpetuated at the bedside.

What’s more, having to deal with caring for these patients after causing delirium with sedation reinforces the idea that the ABCDEF Bundle is impossible to implement because it is “too much work.”
Ironically, it’s the failure to implement these protocols that’s making everything more difficult, as delirium doubles the nursing hours required for care, increases workplace violence, and causes a significant psychological burden for nurses.
But regardless of what the truth may be, when clinicians see the ABCDEF Bundle as extra work, it is less likely to be adapted into ICU patient care.
The reality is until clinicians have the knowledge and support required to prevent and treat delirium, transform patient outcomes, and reduce their workload, it’s unlikely they will ever be empowered or motivated to ensure their patients are awake and mobile.
And when clinicians are deprived of the ability to master these evidence-based practices and truly prevent ICU delirium and ICU-acquired weakness, they continue to suffer from a heavier workload.
But when they adhere to the protocols found in the ABCDEF Bundle, their workload will be lightened, as they’ll be dealing with patients who are more likely to be strong, awake, compliant, and pleasant.
Mobility
Across all disciplines, from physicians and nurses to physical, occupational, and respiratory therapists, early mobility in the ICU is not a standard part of their education.
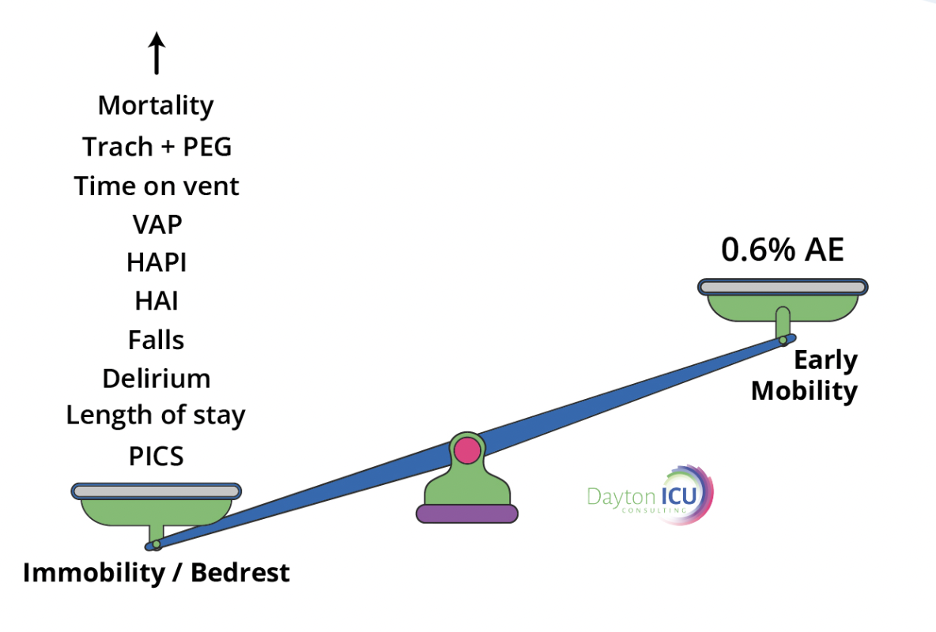
As a result, one of the barriers to early mobility is that many nurses believe their patients are “too sick” to mobilize, as is reflected in this meme:
At the same time, physical and occupational therapists may not have the training and experience to mobilize high-acuity intubated patients with ventilators, and respiratory therapists may be overcome with fear of an endotracheal tube falling out during mobility.
Physicians, on the other hand, may think early mobility is simply passive range of motion and higher levels of mobility are only important after extubation.
But ultimately, until every member of the ICU team understands that early mobility is feasible and safe during critical illness, and has a shared perspective on inclusion criteria, mobility will always be perceived as a scary and seemingly unachievable ideal.
Punitive Safety Culture
In a misguided effort to increase patient safety, a punitive culture has been developing in critical care medicine throughout the years.
Nurses are held solely liable for safety events like falls and unplanned extubations, and this has led to increased sedation, restraints, and confining patients to the bed in the name of “safety.”
Instead of fearing delirium and ICU-acquired weakness, which we know lead to self-extubations and falls in the ICU, nurses are led to believe that patients are “safe” when comatose and strapped to a bed for their entire shift.


The result of all this is that nurses believe their licenses and employment are in jeopardy if patients are awake enough to move or are anywhere but in bed.
However, the truth is that evidence-based practices, like early mobility and cessation of sedation, offer some of the best ways of preventing delirium and ICU-acquired weakness, which can decrease the risk of falls, unplanned extubations, and even violence against health care workers.
When clinicians experience the impact that these protocols have on their workload, safety, and the safety of their patients, they quickly begin to understand that the ABCDEF Bundle brings true safety for everyone, both in the short and long term.
The bottom line is that until clinicians feel empowered and psychologically safe to liberate their patients from sedation, restraints, and the bed, critical care culture cannot transform.
If clinicians aren’t being rewarded for adhering to best practices and protected from a punitive administration, they will continue to choose interventions that allow them control and “safety” during their shift, and it will become increasingly difficult to create Awake and Walking ICUs.
Accountability
Transforming ICU culture and practices requires consistent accountability.
For example, trying to ensure that documentation is accurate can be an incredible challenge.
The current culture in many ICUs encourages poor oversight and low accuracy when screening for delirium and mobility, performing awakening trials, and ensuring reliable RASS scores.
One study showed that despite sedation orders for a RASS 0-(-3), 70% of patients were sedated to a level of -4 and -5, regardless of documented RASS scores of -3 or higher.
Unfortunately, most clinicians don’t know that deep sedation is an independent predictor of mortality and they’re typically not supported in monitoring sedation levels.
Moreover, most clinicians are unaware that a lack of ICU mobility is also an independent predictor of mortality.
It is not standard practice in most ICUs to collaboratively weigh the risks versus the benefits of early mobility, but if early mobility were seen as the life-saving intervention it is, then it would be treated like an antibiotic and never missed.
Yet in most ICUs it is acceptable to chart “bed rest” as a default for all intubated patients as mobility screening.
This causes patients who should be mobilized to easily fall through the cracks, as there is very little oversight for which patients actually have a contraindication to mobility and which patients should be promptly mobilized.
That being said, until the ABCDEF Bundle is implemented, and there is true stewardship and accountability for what’s documented in the ICU, intubated patients will continue to be automatically put on bed rest, and both they and the clinicians who care for them will have to deal with the consequences.
Lack of Interdisciplinary Collaboration
The ABCDEF Bundle is like a team sport – without proper team dynamics, it’s impossible to properly implement these protocols and create Awake and Walking ICUs.
With that in mind, here are some of the interdisciplinary barriers I’ve witnessed in the ICU:
Toxic Hierarchy
When an ICU team has a culture in which physicians are the only decision-makers, idea-generators, and solution-contributors, the entire team suffers.
The ABCDEF Bundle requires that the ICU be a safe place for each member of every discipline to offer insights and ideas that are respected, embraced, and adapted by the entire team.
Each professional is valued and invited to share their expertise.
But when any member of an ICU team feels they have gained all the knowledge they possibly can, and consider themselves an absolute expert, they become impermeable to new information.
They remain unmovable in the practices that are familiar and comfortable to them, and they’re resistant to change and evolution.
Fight for Control
Nurses should not be the only decision-makers when it comes to sedation and mobility practices.
Physicians, respiratory therapists, physical therapists, and all other relevant disciplines must discuss sedation, delirium, and mobility interventions together.
Because when nurses restrict their colleagues from having access to their patients, they also deprive themselves of invaluable assistance with managing things like patient anxiety, delirium, and mobility, which can further exacerbate poor patient outcomes and burdens on nurses.

Interdisciplinary Appreciation
It is key for every member of an ICU team to recognize the value and expertise of their colleagues.
For instance, as nurses and respiratory therapists come to understand, witness, and appreciate the expertise rehab clinicians bring to their patients, they can develop trust and relationships that help optimize patient care and outcomes.
What’s more, when physicians see the safety and skill with which their colleagues handle high-acuity patients, they will be quicker to consult them early on in patients’ critical illness.
Dehumanization
After decades of normalizing constant sedation and immobility, culture in the ICU can easily become dehumanized.
For one thing, when patients are comatose and unresponsive, it’s almost impossible to have a deep human connection with them.
And because clinicians constantly face traumatic and devastating situations in the ICU, ICU culture often teaches us to become “hardened” to protect ourselves from feeling anything that could lead to sadness or burnout.
This emotional distance and posturing can have a decidedly negative impact on an ICU team’s ability to achieve the objective of the ABCDEF Bundle, which is to “produce patients who are more awake, cognitively engaged, and physically active, which ultimately serves to facilitate patient autonomy and the ability to express unmet physical, emotional, and spiritual needs.”
In other words, it is not the culture of most ICUs to want patients to be awake and communicative.
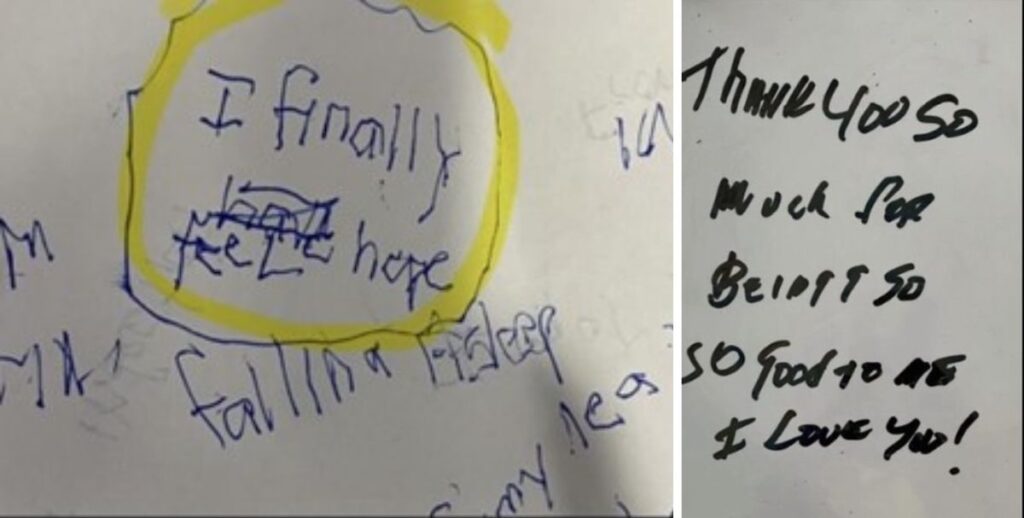
And until ICU clinicians can continually experience the joy of deep connection and communication with their patients, they will never expect this to be the norm:

Ultimately, a RASS score of 0 should be our true goal for most patients in the ICU.
But until we shift ICU culture to look at the patient as an autonomous being who should be awake, communicating, and engaged, with few exceptions, we will not shift our sedation and mobility practices to align with the ABCDEF Bundle.
Final Words
As an ICU revolutionist, you shouldn’t have to endure such challenging dynamics and moral injury when all you’re trying to do is advocate for the use of best practices for your patients.
Luckily, when the rest of your colleagues receive the key foundational knowledge that’s required to understand the risks and costs of sedation and immobility, they will be much more open to new skills, dynamics, and relationships that will help transform sedation and mobility practices.
As an ICU consultant who helps clinicians create Awake and Walking ICUs, some of my favorite feedback from ICU teams, following their evolution, has been:
- “This is so much easier!”
- “We’re finally working together as a team.”
- “I am really enjoying my new friendships with my PTs, OTs, RTs, etc.”
- “The morale of the unit has really changed since we’ve started having a lot of patient success. We can see that we’re saving lives and we’re celebrating together.”
If your team is ready to overhaul its culture and practices, please don’t hesitate to sign up for a free consultation.




