Back when I was studying to become a nurse, I had an experience in the ICU that changed me forever.
As a starry-eyed 18-year-old nursing student, I was incredibly excited to finally be in the ICU, experiencing what I’d dreamed about for so many years.
But when I got there and started to learn what ICU culture is really like, it broke my heart.
At the time, I was pretty chatty, not least because of how excited I was, and the nurse I was shadowing definitely wasn’t a fan.
Eventually, she turned to me and said, “I work here in the ICU so I don’t have to talk to anyone. So, if you’re thinking this is going to be your social hour, you’re wrong.”
Now, I’m not saying that all ICU clinicians are like this, but this is the kind of attitude that ICU culture tends to create, and over the years, not much has changed.
The fact is most ICU clinicians are taught that the most humane thing they can do for patients is to keep them heavily sedated, and as a result, communication in the ICU between clinicians and patients is almost non-existent, as the patients are usually comatose.
But the truth is avoiding communication in the ICU isn’t in anyone’s best interests, and for the most part, keeping patients heavily sedated actually does more harm than good.
Among other things, these practices make clinicians’ jobs harder, erode the health and autonomy of patients, and preclude family involvement.
So, in an effort to set the record straight on communication in the ICU, I wanted to publish an article exploring why this aspect of ICU patient care is so broken, how these shortcomings can affect everyone involved, and what clinicians can do to improve ICU communication.
If you’d like to learn more about communication in the ICU, you can check out Episode 103 of my Walking Home From The ICU podcast.
Why Is Communication in the ICU so Broken?
When I work with ICU teams to help them improve sedation and mobility practices, I find that most ICU clinicians are pretty much lost when it comes to communication.
Often, they’ll ask me questions like, “Okay, now they’re awake. How do we do this?” offering a poignant reminder of how ill-equipped most clinicians are when it comes to communication in the ICU.
But why is this?
Well, aside from the prevailing ICU culture, which teaches clinicians that the best thing they can do for their patients is to keep them heavily sedated, clinicians just aren’t given the training or tools they need for effective communication in the intensive care unit.
For the most part, ICU clinicians don’t expect to have to converse with patients because they’re all too sedated to communicate.
Moreover, ICU teams are not used to taking the patient’s input into consideration when assessing them, or in any way involving them in decisions about the care they’re receiving.
This changes the way that clinicians view their patients, and has a demonstrably dehumanizing effect, as the patient’s wishes aren’t even taken into consideration, much less solicited.
For example, many nurses aren’t even aware of the importance of having a whiteboard or pen and paper in each room, let alone knowing they can contact those who work in speech therapy for help.
As a result, speech therapists typically only come to the ICU to do swallow evaluations after patients have been extubated. And rarely, if ever, are they called in to help clinicians with communication issues.
Why Is Communication in the ICU so Important?

The United Nations Universal Declaration of Human Rights states that communication is a basic human right, but that only scratches the surface of why communication in the ICU is so important.
For a patient, effective communication in the intensive care unit means everything, as it allows them to have autonomy, dignity, control, connection, and comfort.
At the same time, it keeps them cognitively engaged, helps to prevent delirium, and allows them to be properly informed, have their wishes respected, and communicate their spiritual, physical, and emotional needs.
For families, communication in the ICU allows them to converse with and comfort loved ones, and avoid situations where family members have to make life-changing decisions on behalf of patients without their input.
As a clinician, knowing how to effectively communicate in the ICU just makes everything easier, and mitigates the dehumanizing effect of ICU culture.
It allows you to take less time to assess patients, improves patient safety and compliance, and gives you the chance to develop relationships with patients and build trust by answering their questions and helping them to understand the situations they face.
What Are the Consequences of This Lack of Communication in the ICU?
Lack of communication in the ICU can create dire consequences for clinicians, patients, and their families.
If you’re a patient, this lack of communication can result in trauma, frustration, anxiety, agitation, and delirium, and it also results in patients dealing with unmet needs and suffering from undiagnosed changes.
For example, one of my podcast listeners shared an anecdote with me about one of their patients.
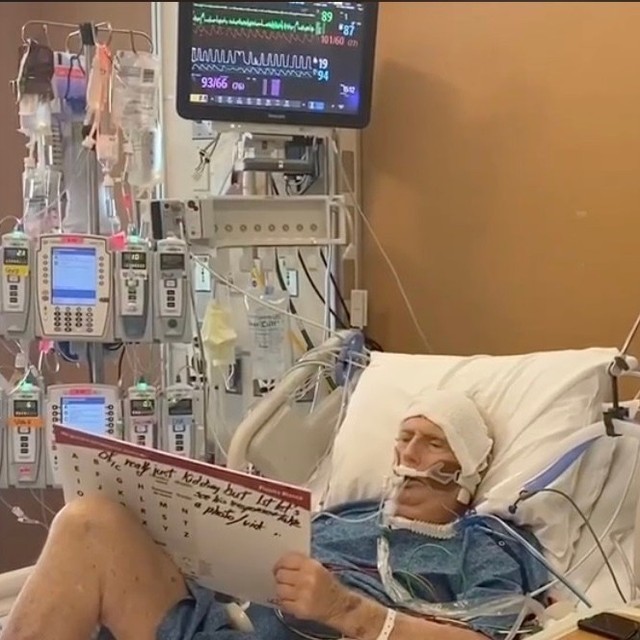
This patient was intubated, but the ICU where they were being treated chose to adhere to evidence-based practices and kept them awake while on the ventilator.
And because they were awake, the patient was able to tell them that they were having chest pain.
At this point, they went ahead and did an x-ray on the patient’s chest, only to find out that they had a pneumothorax. Then, as they were looking at the x-ray, the patient went into respiratory arrest and their heart stopped.
This shows just how important communication in the ICU is, because as a result of the patient being able to communicate, clinicians knew there was something wrong, and were able to find out what it was by taking an x-ray.
More importantly, this also allowed them to save this patient’s life.
But if they’d been unable to speak, clinicians may have never known anything was wrong, wouldn’t have thought to take an x-ray, wouldn’t have known what was causing the patient’s respiratory arrest, and it may have been too late for them to do anything.
At the very least, even if they were able to save the patient, they would have wasted a lot of time figuring out what was causing this to happen. This would have made everything more difficult, not least because it would significantly reduce the patient’s chances of survival.
This lack of effective communication in the intensive care unit can also create serious consequences for patients’ families, as they may have to make gut-wrenching decisions on their behalf, and are otherwise unable to communicate with them during what could be the last moments of their life.
Last but not least, this lack of communication in the ICU can also pose serious problems for clinicians.
For instance, if patients are unable to communicate, it will take much longer to assess them, and this can result in a ton of frustration for clinicians, who have many other patients to see, and don’t have a lot of time to deal with this sort of thing.
This also creates a situation where clinicians will be more inclined to sedate patients, as they’re more likely to become agitated when they can’t communicate, and this makes working conditions less safe.
Furthermore, this all perpetuates the idea that patients can’t be awake and calm on the ventilator, which is one of the things about ICU culture that we desperately need to change.
When it Comes to Communication in the ICU, What Needs to Change?
First and foremost, if we want to improve communication in the ICU, ICU culture needs to change, along with the mindsets of those who work in the ICU.
Instead of avoiding communication with patients, and clinging to the erroneous belief that this makes our jobs easier, we need to fight for patient autonomy.
If we ever want to get out of the situation we’re currently in, these are the kinds of ideas that need to prevail in ICU culture.
ICU clinicians need to be much more concerned with the best interests of the patient, rather than just focusing on what they know, what they’re most comfortable or familiar with, or what’s most convenient for them. And they need to realize that this lack of communication only makes their jobs harder.
At the same time, if families get more engaged and involved with what’s happening to their family members in the ICU, things are bound to change.
Families should demand that their loved ones be able to communicate, and oftentimes, they’re the ones who’ll have to sit there and spend whatever time is necessary to figure out what they’re trying to say and what they want, so family involvement is also key to the resolution of this issue.
What Can Clinicians Do to Improve Communication in the ICU?
I know this seems daunting, but the truth is there are several simple solutions that can be employed in every ICU to improve communication with patients.
Here are some things I like to recommend to ICU clinicians who want to improve their communication:
- VidaTalk – This app allows clinicians to communicate with non-verbal patients or those who are otherwise dealing with communication barriers. This software is also a reimbursable intervention, and for each patient who uses it, your hospital can get $1,000 through Medicare or Medicaid.
- Paper, pens, and pencils – One of the most effective ways to communicate with non-verbal patients is to allow them to write things down. They may not seem like much, but these items can have a huge impact on communication in the ICU.
- Whiteboards or Boogie Boards – Paper takes up a lot of space, and if you’re using a lot of it, it can get expensive. With that in mind, these items offer a great alternative to communicating via pen and paper.
- Laptops, tablets, or cell phones – These kinds of devices are absolutely invaluable when it comes to non-verbal communication, so it’s always good to have at least a few on hand in your ICU.
- Passy Muir valves – These valves allow patients with tracheostomies to talk by redirecting airflow through the mouth, nose, and vocal folds.
Do you want to improve communication between patients and clinicians in your ICU? We can walk you through the entire process, so please don’t hesitate to contact us.



 I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.
I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.
