“Let’s introduce the bundle gradually. We don’t want to overwhelm anyone. Let’s see what the team is willing to do. We can start with awakening and breathing trials, then tackle the rest once we have those down.”
This kind of conversation has echoed through medical organizations and clinical leadership teams for years.
It’s a logical approach, especially for those who are trying to change their ICU’s culture, and working to prioritize awakening and mobility, rather than just automatically sedating intubated patients.
This type of change must be strategic and safe.
But is ABCDEF Bundle implementation, done “one letter at a time” truly the safest and most effective pathway?
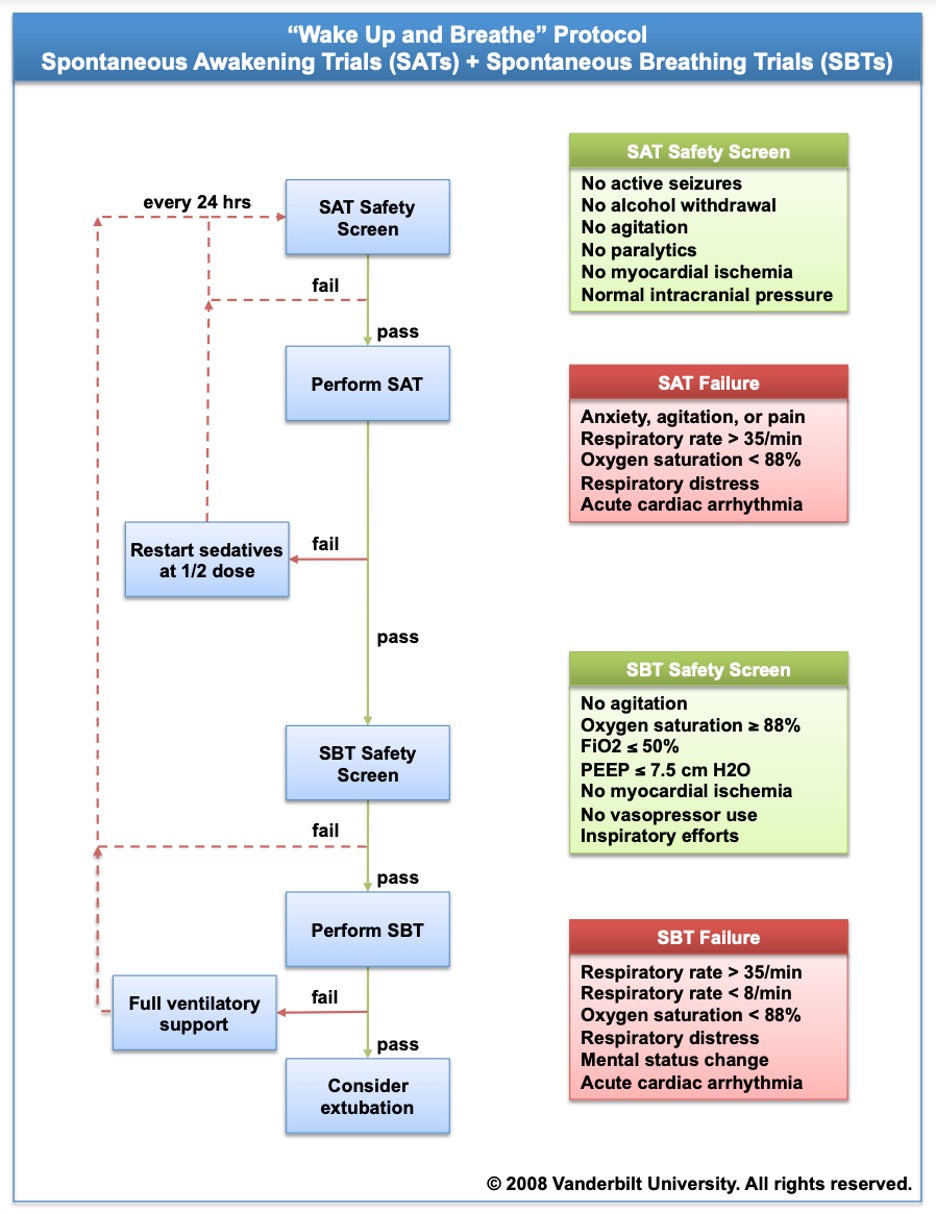
Since 2008, we’ve been “starting with Spontaneous Awakening Trials (SATs) and Spontaneous Breathing Trials (SBTs).”
We know that implementing SATs and SBTs significantly reduces ventilation time and improves survival rates compared to continuous sedation. The evidence is clear: These practices lead to fewer patient complications.
But are we doing the best we possibly can for our patients?
With that question in mind, consider these impactful statistics:
- Mobilizing patients within 48 hours post-intubation can increase their chances of going home by 24%, reduce delirium duration by two days, and enhance cognitive function by 20% per year after discharge.
- A lack of mobility in the ICU results in higher rates of readmission and mortality within the first year after discharge.
- For every additional 10 minutes of mobility, there’s a corresponding 1.2-day reduction in length of hospital stay.
- ICU mobility can decrease hospital readmission rates by a staggering 59%.
- The inability to stand three months post-ICU discharge increases the risk of mortality by 4.2 times in the first year.
- Mobility during mechanical ventilation, even with an endotracheal tube in place, is remarkably safe, with an adverse event rate of just 0.6%.
Given these proven benefits for both patient outcomes and cost savings, how prevalent is early mobility in the ICU?
And does starting “slow” with just awakening and breathing trials really pave the way for successful early mobility?
A German study, published in 2014, revealed that only 24% of ICU patients were mobilized out of bed, with a mere 8% of intubated patients receiving the same treatment.
The first ABCDEF Bundle rollout, published in 2019, showed high compliance for SATs and SBTs among more than 15,000 patients across 68 facilities, yet only 12% of patients got up on their feet.
Most recently, a 2025 report covering 135 ICUs across 54 countries found that less than 10% of intubated patients were mobilized.
And after training 13 ICU teams and connecting with many more worldwide, I believe that “starting slow” might actually be creating a “failure to launch.”
As my friend, Margaret Arnold, aptly put it, trying to ease into an early mobility program is akin to water-skiing with your skis stuck halfway in the water.
Because if you never fully commit and get on top of the water, you’ll quickly exhaust yourself from battling the resistance.
For those who haven’t been at the bedside conducting awakening trials, let me clarify this further.
Starting continuous sedation is like pulling the pin from a grenade, and in many ICUs, this practice gets perpetuated from shift to shift without being re-evaluated.

And as you can see in the image below, SATs and SBTs are found on the same page in publications and taught as interdependent, and as a result, sedation often isn’t revisited until ventilator settings are at a minimum and all signs of critical illness appear to have resolved.
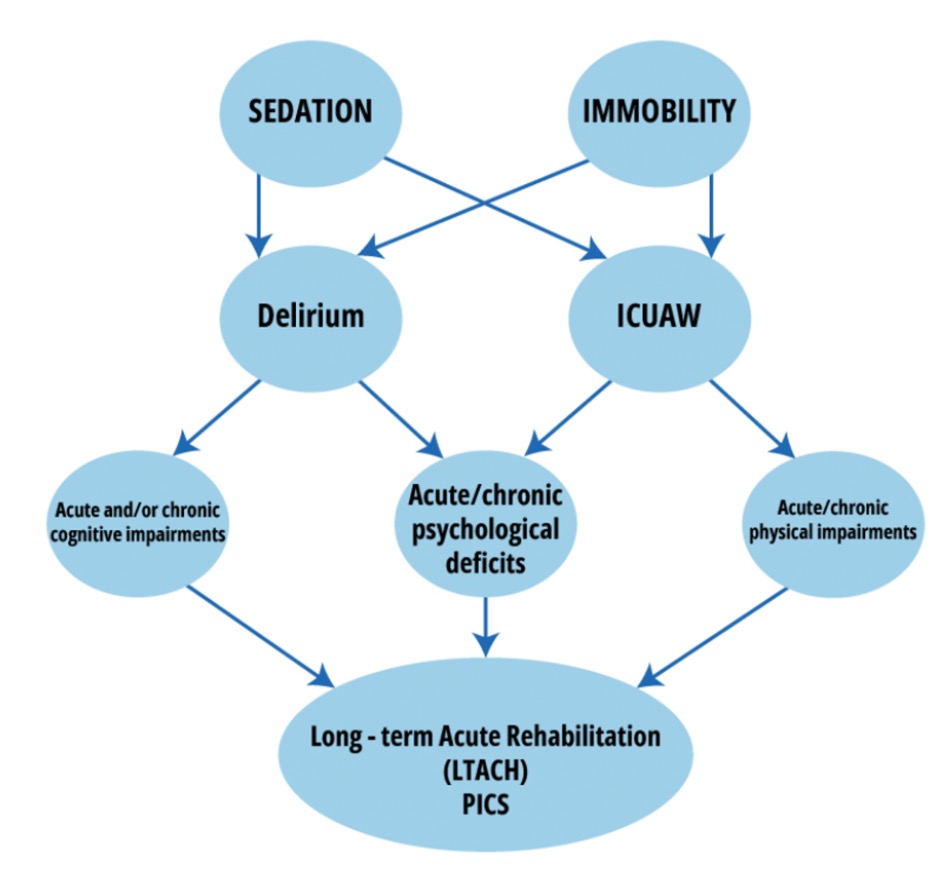
Consequently, patients may remain restrained and sedated in bed for days, leading to a staggering 3,095% increased risk of delirium if sedation continues beyond seven days.
In any case, each day of delirium corresponds to a 10% increased risk of death.
And while there might be a daily on-and-off toggle for sedation, it rarely aims to maintain patients in a fully awake state that promotes autonomy, mobility, or even communication.
The Hard Truth of ABCDEF Bundle Implementation
Continuous sedation increases the risk of delirium by an alarming 226%.
So, when sedation is finally turned off for a SAT, patients often emerge anxious, restless, and even panicked.
The terrifying experiences they’ve endured while sedated come rushing back, and as a result, restraints may be applied, and sedation resumes – leading to devastating outcomes.
This sequence of events is one of the main reasons why ABCDEF Bundle implementation fails.
This is echoed in findings from the recent TEAM trial, and as I discussed in Episode 117 of my Walking Home From The ICU podcast, this trial identified sedation and agitation as the primary barriers to mobility after six days of sedation.

We must recognize that by clinging to the outdated practice of automatically sedating patients post-intubation, we inadvertently create obstacles to their mobility.
This exacerbates delirium and ICU-acquired weakness, complicating mobility efforts significantly.
All things considered, we must stop treating the ABCDEF Bundle as nothing more than a sequential checklist.
Instead, we must view it for what it is – a collection of evidence-based practices that are most effective at enhancing patient outcomes when performed together.
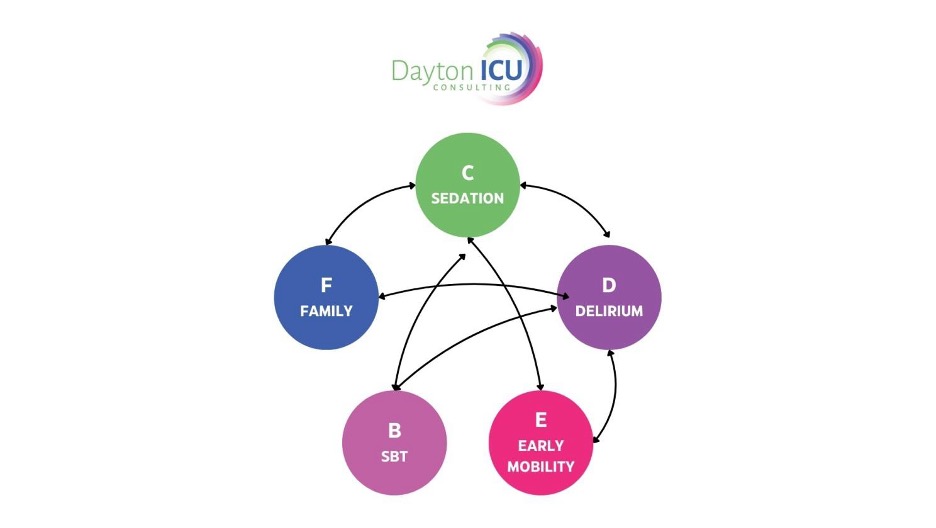
The truth is, practicing the Bundle letter by letter is simply not feasible, as each component is interconnected and reliant on at least two other elements. For example:
“A” for Assessing, Preventing, and Treating Pain
Sedation often restrains patients chemically, making it difficult for them to articulate or express their pain.
That being said, the “A” in ABCDEF Bundle flourishes when patients are awake, cognitively engaged, and empowered to communicate the severity, type, and location of their discomfort.
“C” for Choice of Sedation and Analgesia
Keeping patients awake while intubated is challenging if they’re not mobilized to address anxiety, pain, tube tolerance, and prevent or manage delirium.
As such, the “C” in ABCDEF Bundle prompts us to critically evaluate whether sedation is even necessary.
“D” for Assessing, Preventing, and Treating Delirium
Properly addressing delirium is impossible when patients are routinely given sedatives that can induce delirium, leaving them unable to mobilize or engage with family members.
Once delirium sets in, awakening trials become arduous as patients may exhibit confusion, impulsivity, and are 11.6 times more likely to self-extubate.
Their heightened anxiety can also lead to tachypnea, causing failed breathing trials.
“F” for Family Engagement
It’s tough for families to connect with and support patients who are chemically restrained, unresponsive, and unable to convey their needs.
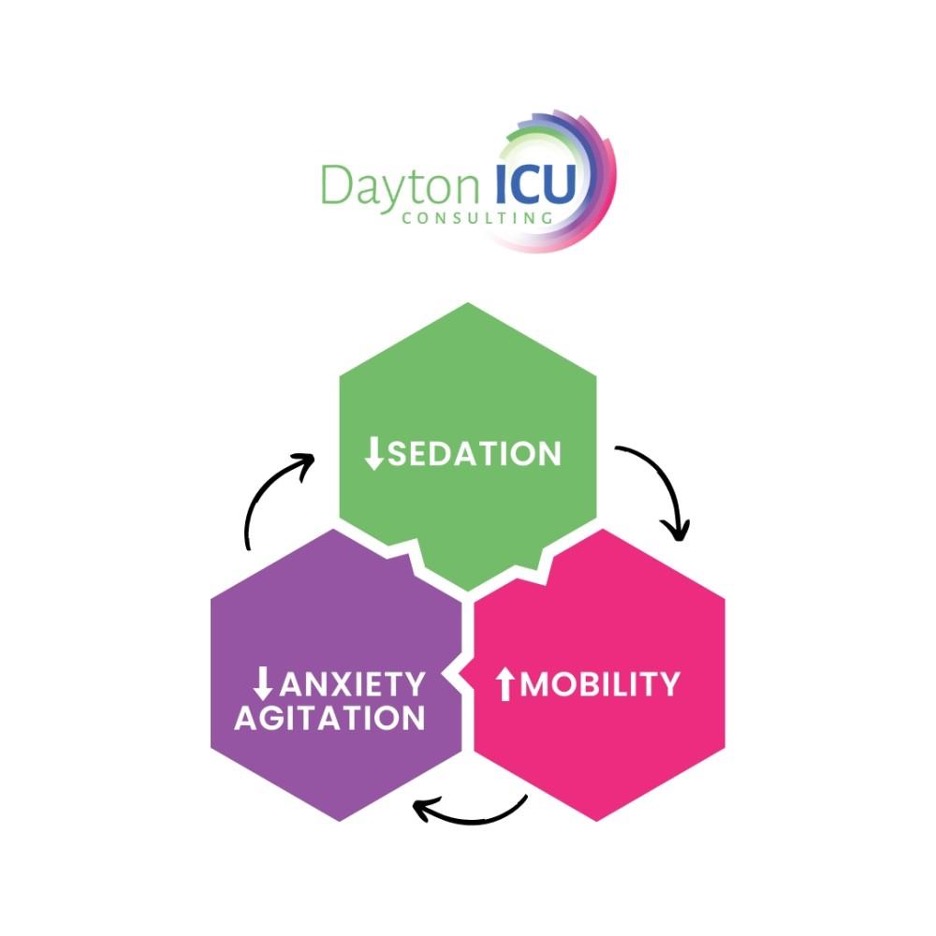
But by avoiding sedation, we can mobilize patients promptly, thus preventing and treating delirium.
This, in turn, often reduces anxiety and agitation, protecting patients from the cycle of starting and resuming sedation.
And regardless of what perspective we choose to take on this issue, the fact of the matter is, if we cling to automatic sedation and continue with traditional approaches to SATs and SBTs, we will inevitably struggle with ABCDEF Bundle implementation.
If we delay the cessation of sedation until we evaluate for extubation, or treat SATs like vacations, breaks, interruptions, or holidays, we will find ourselves contending with issues like delirium and ICU-acquired weakness.
As a result of this lack of proper ABCDEF Bundle implementation, clinicians will say things like:
- “Patients will self-extubate if we don’t sedate them.”
- “Our patients are ‘too sick’ to be mobilized.”
- “We don’t have enough staff for early mobility.”
To be fair, in the current ICU landscape, we may not have sufficient staff to mobilize every patient in a unit filled with delirious and weakened individuals.
Furthermore, we must acknowledge that keeping patients on ventilators and hospitalized for extended periods of time – only to later readmit them – places a burden on our resources, which are already stretched thin.
From my personal experience, and through the teams I’ve trained, I’ve observed that when health care teams prioritize keeping every patient awake and communicative shortly after intubation, they encounter far fewer challenges with agitation, as they do during traditional awakening trials.
Mobilizing patients within 12 to 24 hours of intubation enables them to move independently, follow commands, and engage meaningfully with their care teams.
What’s more, the incidence of delirium and ICU-acquired weakness significantly decreases, and staff often say things like, “Wow, this is so much easier. I really love this!”
With that in mind, I encourage you to listen to several episodes of my Walking Home From The ICU podcast, including:
- Episode 178: The Power of Nursing Leadership to Revolutionize the ICU, which features assistant nurse manager, Andrea Silva, BSN, RN, who shares her journey toward revolutionizing care in her ICU.
- Episode 185: The ICU Revolution at Mercy San Juan Medical Center Part 4, featuring nurses from the Mercy San Juan trauma ICU, who explain how keeping patients awake and mobile has impacted their career fulfillment and team dynamics.
- Episode 38: “THEY’RE AWAKE?!?” and Episode 114: From the Eyes of a Travel Nurse, which both feature travel nurses who compare their workloads in Awake and Walking ICUs to that of “normal ICUs” during COVID-19.
The insights offered in these episodes confirm that preventing delirium and ICU-acquired weakness is far simpler than treating these issues after the fact, and what we do at the onset of critical illness profoundly influences subsequent outcomes and workload.
Ultimately, until we master the art of keeping patients awake and mobile early on, we will miss out on the joy, success, and ease that the ABCDEF Bundle can truly offer.
Do you need help with ABCDEF Bundle implementation? If you’re ready to create an Awake and Walking ICU, please don’t hesitate to book a free consultation.



 I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.
I stumbled upon Kali’s podcast midway through my anesthesia critical care fellowship in February 2021. At our institution, I got the impression that patients in the ICU either got better on their own or had a prolonged and complicated course to LTAC or death. In her podcast, Kali explained that LTAC was rarely the outcome for patients in the Awake and Walking ICU in Salt Lake City.
