Medicine is a field of evolution with a continuous trajectory of exploration, discovery, change, and progress.
And this perpetual pattern has been just as reliable as the predictable resistance that comes with change.
Past Revolutionists Who Fought to Humanize Critical Care
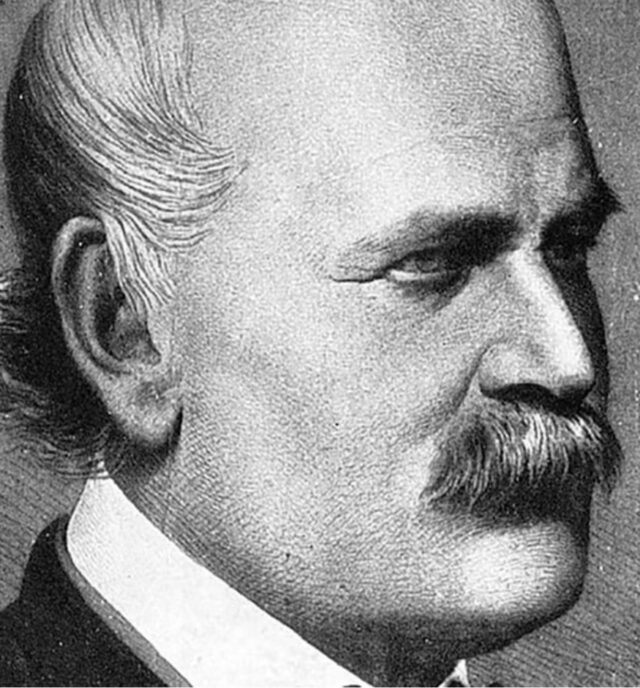
This was demonstrated in the journey of Ignaz Semmelweis (pictured above), a Hungarian physician who, in 1850, proposed that birthing mothers were dying from contaminants carried by physicians from cadavers of study to mothers.
Semmelweis was met with refusal to consider that long-held practices were causing patient harm and death.
As a result, he was removed from his position and was suspected to be driven to “madness” as he toured throughout Europe teaching and begging physicians to wash their hands.
He later died of sepsis in an insane asylum.
Elizabeth Kenny (pictured below) found similar opposition when she proposed that children with polio be treated with massage and movement for affected limbs rather than casts and immobilization.
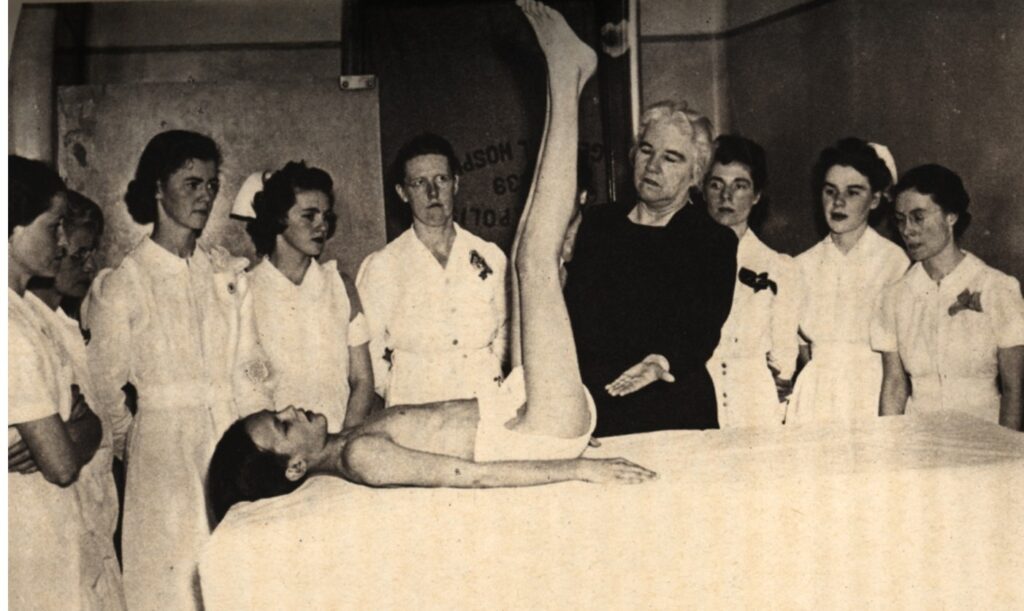
Instead of eagerly accepting new interventions that would save lives and physical function, physicians were threatened and defensive in response to a female nurse’s disputation of their treatments.
Nonetheless, Kenny remained outspoken in advocating for the treatment she knew was right. She was said to be a “raging tiger and merciful angel.”
Eventually, she left the resistance in Australia and came to the United States to start “Kenny Clinics” to treat polio patients using her unique method.
She personally treated over 7,000 children and influenced the care of many thousands more through education and opposition to standard treatment.
The Revolutionists of Today
Even today, after decades of fighting standardized automatic sedation and immobility for all intubated patients, ICU revolutionists are facing similar barriers.
Despite decades of research revealing the harm of sedation and immobility, and evidence showing the benefits of the ABCDEF Bundle, change has been an ongoing battle.
Still, the research clearly shows that when it’s implemented in the way it was intended, the ABCDEF Bundle decreases hospital costs by 30%, 7-day mortality by 68%, delirium by 50%, and hospital readmissions by 46%, while increasing discharges straight home by 36%.
As was revealed in Episode 197 of my Walking Home From The ICU podcast, clinicians who dare to go against cultural norms to give patients the ability to communicate, be informed and autonomous, and mobilize while intubated, face incredible opposition.
ICU revolutionists are demeaned by superiors, bullied and threatened by colleagues, and some nearly lose their jobs in response to them attempting to challenge the status quo by:
- Asking questions about sedation and mobility
- Mobilizing patients that are appropriate for mobility
- Educating families about delirium, mobility, and post-ICU syndrome
- Having patients awake and writing on clipboards against colleagues’ preferences
I invite you to listen to this podcast to hear stories from numerous revolutionists who’ve shared their experiences attempting to humanize critical care by advocating for evidence-based practices.
Below you’ll find a particularly poignant example of this, from an occupational therapist, which I shared in the episode:
“I’m an OT and have been very steadfast in trying to promote change, even if it’s minimal. We must start somewhere. Recently, myself and two PTs were recognized by a trauma surgeon for helping get a patient extubated, whom they were adamant would be trached, PEGed, and sent to LTACH.
“I coordinated the sedation, medication, vent, weaning, and family present for two days after being intubated and sedated with no SAT/SBT for five days with a doctor who then held nursing and RT accountable to the plan.
“He sent a very thoughtful email to upper-level management about the efforts that were made, the confidence in pushing normal boundaries, the outstanding impact that it had on patient outcomes and requested consistent presence in our MSICU.
“I was never told about this email from my boss. Instead, myself and the two PTs who helped with this co-treat were pulled into a meeting and reprimanded for going ‘outside our scope of practice,’ not following the chain of command, going to the MD over the RN, telling nursing what to do, not including RT in the session, et cetera, et cetera.
“They told us we are arrogant thinking we know more than anyone else, and that ‘it’s not just about what the research says.’ They said change takes years. They explained that the upper-level management from multiple departments, including themselves, do not understand the ABCDEF Bundle or ‘believe in it.’
“So, we cannot continue in this manner, or no one will want to work with us. Since this meeting, myself and those two PTs have been pulled off the ICU to staff the floors.
“They have placed novice and new grad therapists in the ICU, instead, who are not comfortable with early mobility on critically ill or ventilated patients because they are ‘licensed clinicians and understand what is safe, even if it’s bed level.’
“Those therapists would never have a challenging conversation or push any boundary because they simply are not experienced enough to have it. They do as they’re told by nursing and keep their day moving instead of advocating for the patient and what is right.
“Talk about burnout. I ask myself daily how much longer I’m going to be able to keep up with this. I got a written warning for explaining to a nurse that it was okay for therapy to work with someone on 0.4 of Precedex (they were not even intubated) and educating on sedation use, delirium, and preventing ICU weakness because ‘sedation isn’t my scope of practice’ and if the nurse says ‘no’ I should just write a ‘hold,’ not prove that I’m right.
“I was initially hired because of my ICU experience, and this hospital has just built a critical care tower with 78 beds. I have done countless lunch and learns with the therapy department, created resources, provided one-on-one training for comfortability, developed the therapy ICU competency, and so much more over the last two years.
“There’s no internal drive and no external motivators at this place, and people just simply do not care. There’s no incentive to learn.
“I went into health care to help people. I am now questioning my morals and values at the end of the day instead.”
It is astounding to consider that a clinician who orchestrated teamwork and guided collaboration to implement evidence-based best practices that resulted in a patient being spared a tracheostomy and extensive rehabilitation would be kicked out of the ICU by their leadership.
But this is by no means the only example of this sort of behavior.
In Episode 94 of my Walking Home From The ICU podcast, a nurse from an Awake and Walking ICU, who started working in a new ICU, was yelled at in the hallways in front of her entire team for sitting her intubated patients at the side of the bed and Zoom-calling their families during COVID.
Eventually, they stopped assigning her intubated patients because they didn’t like her having the patients awake and moving.
Another revolutionist received a severe written “counseling” for teaching families about delirium, immobility, sedation, and post-ICU syndrome.
The rest of the team did not want that information to be disclosed to families, as they were upset that families would be aware of the risks of these interventions and preparing for post-ICU life.
She was warned to never broach these topics with families again.
Throughout the years, I have been in contact with over a dozen revolutionists who have either changed hospitals or left critical care medicine entirely due to the moral injury of witnessing preventable patient harm and being restrained from protecting or helping them.
In Episode 166 of Walking Home From The ICU, a pharmacist with 10 years of critical care experience left because the hospital’s chief nursing officer banned her from talking about sedation during rounds, as it was upsetting the nurses to have to discuss RASS levels and awakening trials.
During one of her final shifts, she exclaimed, “We are killing these people!”
She then took her vast knowledge, expertise, and compassion – and left critical care.
Another example of this can be found in Episode 156, when I discussed a seasoned acute care nurse who entered a new critical care position with knowledge about the ABCDEF Bundle.
During her orientation period, she was repeatedly pulled into her manager’s office for being “unteachable” due to her charting a RASS that was lower than what her preceptor wanted her to chart, turning sedation off for an awakening trial rather than just slightly down, asking about mobility, et cetera.
After a few months of watching patient harm, she gave up on her dream of working in the ICU once she realized she couldn’t tolerate that level of moral injury.
I am inspired by the brave revolutionists who bring the evidence to their clinical leadership to say, “I am willing and ready to work hard to bring these changes that will save lives, millions of dollars, and fix a lot of the problems our hospital is worried about right now.”
It is demoralizing to hear how many are met with the response, “That’s really nice, but it’s not a priority right now,” or “Things are fine the way they are.”
Some of the most lethal words in medicine are “This is how we’ve always done it.”
Yet, that is the common rebuttal revolutionists receive.
They are seen as “troublemakers,” “delusional,” and “difficult to work with.”
This ignorance, fear, resistance, and hostility is creating toxic work environments and increasing the burnout and burden on our clinicians.
Upon hearing Episode 197, which I referenced above, another revolutionist said, “That episode is making me see red. I am SEETHING. It is the Santa Claus effect; I cannot go back and cannot think of how we would still be breaking our back with total care on sedated patients.”
To the revolutionists out there: Keep going. You are not alone. Every 10% improvement in compliance with the ABCDEF Bundle improves survival by 15%. You are saving lives.
And may we continue to be raging tigers and merciful angels by fighting to give patients the best chance to survive and thrive.
Want to connect with clinicians who are fighting to humanize critical care? Join our monthly meetings for ICU Revolutionists to gain support from fellow clinicians from around the world.




