Consulting for Medical Professionals

You entered critical care medicine because you want to save lives. But when it comes to sedation, mobility, and the prevention and management of delirium in the ICU, the methods used in most intensive care units are not aligned with best practices, such as the ABCDEF Bundle.
These outdated standards can create a situation where patients are less likely to survive and unlikely to thrive. In addition, they also create a more dangerous environment for your staff and one that’s more likely to induce burnout and lower the morale of your team. Moreover, these antiquated standards are less cost-effective and leave you more vulnerable to litigation, as your patients aren’t receiving the best possible standard of care.
Every healthcare consultant on our team has the expertise to help you modernize critical care methods in your ICU, bringing them into alignment with the latest research by implementing evidence-based best practices. This will ensure better outcomes for your patients and a better working environment for your staff, as well as decreased risk of litigation.
We can provide on-site support and education from a dedicated healthcare consultant who will empower and equip you and your team with the right knowledge and tools to implement the most humane standards of care, including making the transition to an Awake and Walking ICU.
Through our services, you will be able to:
- Decrease costs and eliminate waste
- Increase the survival rate of your patients
- Create a safer environment for your team
- Ensure more interdisciplinary collaboration
Through our services, you will be able to:
- Reduce burnout and improve the morale of your staff
- Implement the most up-to-date, cost-effective practices
- Formulate evidence-based sedation and mobility protocols
- Maximize insurance and Medicare/Medicaid reimbursements
- Decrease patients’ chances of suffering from hospital-acquired complications
Overview of On-Site Consulting
Thank you for taking an interest in helping your team to improve sedation and mobility practices!
The objective of our consulting services is to provide each and every member of your team with the knowledge and tools they need to contribute to the creation of an Awake and Walking ICU, where sedation and immobility are only implemented when absolutely necessary, for the shortest possible duration, and with immediate rehabilitation, if possible.
We provide the knowledge and practical skills clinicians need to critically think through delirium, sedation, and mobility management as part of a collaborative team for each patient.
Our consulting services involve both a series of webinars, and on-site support, where we work with your team to do simulation training and offer guidance on current patients.
Webinar Presentations
Before we come to your ICU and work with you in person, it’s important that every member of your team has participated in the following four webinars. This will give them the background knowledge they need to understand the urgency of implementing evidence-based sedation and mobility practices.
This also allows us to be more efficient in our consulting, as your entire team will understand the basics and everyone will be on the same page before we even start the in-person training.
To ensure we can be as productive as possible during our time on site, we encourage every member of your team to participate in the following four webinars before we arrive:
Introduction to an Awake and Walking ICU
The realities of deep sedation and immobility for every patient on mechanical ventilation are clearly addressed. Research on ICU delirium treatment, ICU-acquired weakness, post-ICU PTSD, post-ICU dementia, prolonged time on the ventilator, and mortality related to sedation and immobility practices are applied to real case studies.
Pictures, videos, and case studies will demonstrate the drastic difference in outcomes seen in an Awake and Walking ICU. ICU team members will gain an understanding of the gaps in our ICU culture and practices and will have a shift in perspective on what is possible and what is vital when it comes to ICU patient care.
Diving Deep into Delirium:
This presentation addresses all the causes of delirium, as well as the risks of each common sedative used in the ICU. The increased workload, financial burden, and impact on patient outcomes of delirium are presented. Your team will hear about the role of family and mobility in the prevention and treatment of delirium.
Videos from survivors of sedation and delirium show what it was like under sedation and what life with post-ICU PTSD and post-ICU dementia is like for them now.
Mobility is a Life-Saving Intervention
The history of bed rest, the inter-organ connection between the muscles and other systems, and the impact of muscular atrophy on critical illness are shared. The effect of ICU-acquired weakness and diaphragm dysfunction on the rates of death, disability, tracheostomy, and time on the ventilator is revealed.
In this talk, your audience will hear about survivors who discuss their rehabilitation and the life-long impact of ICU-acquired weakness. Research on the safety, feasibility, and efficacy of early mobility is also shared. The science behind the benefits of each level of mobility is explained.
After participating in this presentation, ICU team members will understand mobility as a life-saving intervention, and clinicians will learn to prioritize prompt mobility as a part of best practices.
Questions and Answers
After collecting questions from a pre-survey, clinicians will meet with experts from their own field as we discuss the role each discipline plays in an Awake and Walking ICU. Live questions and discussions will be welcomed to ensure each team member is empowered with the knowledge and tools they need to effectively play their part on the team.
Please note: These webinars are recorded and can be loaded onto your learning platform for indefinite use. This allows the opportunity for all members of your team to participate and can help to onboard future clinicians to ensure continuity of culture. They can also be used for continuing education credits.
On-Site Visits
Once your team has participated in the webinars and understands the why behind evidence-based sedation and mobility protocols, then they will be ready to learn and practice the how.
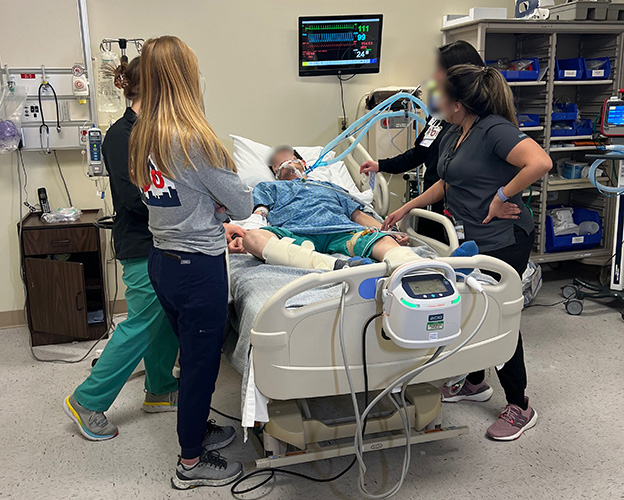
The goal of the on-site visit is to provide clinicians with the opportunity to participate in simulation training and receive support for current patient cases.
Our team will spend four or five days with your team during day and night shifts. This will allow us to observe team dynamics, workflow, and identify possible barriers. We will strive to understand the culture of your ICU and help formulate solutions to fit your needs.
We will attend rounds and participate as much as your team is comfortable with. We can offer ideas and suggestions, facilitate collaboration, and share experiences and insights applicable to your current patients.
Although we’re unable to personally touch the patients, we can be at the bedside with the clinicians and help them through their process of care.
Our time on-site also allows us to personally meet with members of each discipline such as pharmacists, dietitians, nursing informatics, administration, etc. to secure greater buy-in and collaboration.
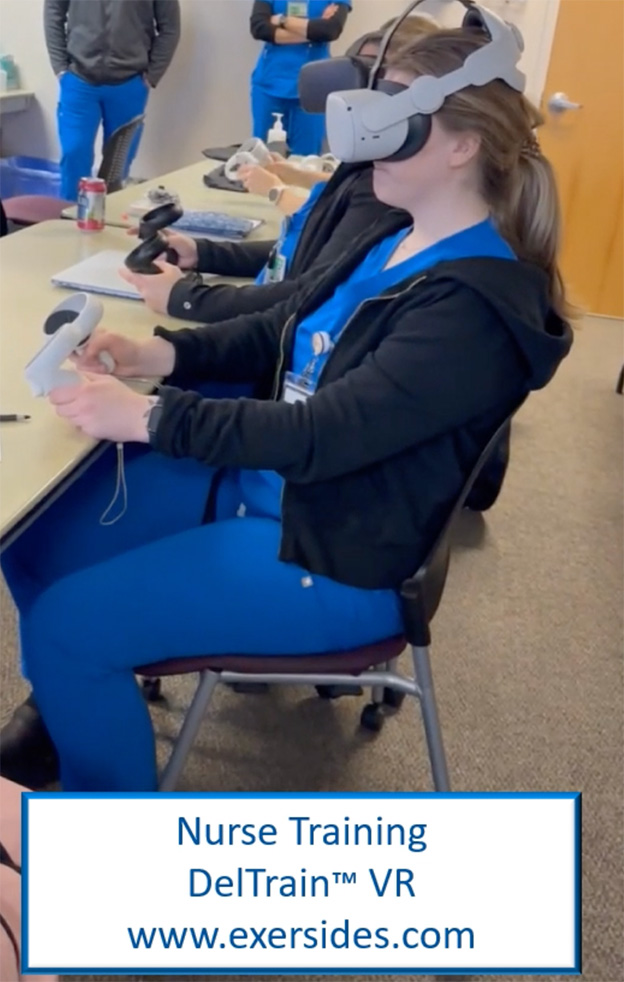
In addition, we also provide time with a VR (virtual reality) program that puts participants into the perspective of the patient during delirium, sedation, awakening trials, mobility, and more, which helps to create empathy and gives clinicians a better understanding of what patients have to endure.
These services also include tools for sustaining this change, such as family education packets, communication and agitation toolkits, etc., which are all adaptable for your unit’s nuances and needs.
This time with your team will result in improved buy-in, excitement, perspective, confidence, skills, and personal experiences that will help your team to create and sustain an Awake and Walking ICU.